NCLEX - Ischemic Heart Disease Pathophysiology
Start your One-Week Free Trial
Already subscribed? Log in »
Here are key facts for NCLEX RN Examination from the Ischemic Heart Disease tutorial, focusing on essential nursing concepts, patient assessment, and clinical considerations, as well as points of interest at the end that are not directly addressed in this tutorial but should help you prepare for the boards. See the tutorial notes for further details and relevant links.
 Below is additional information important for NCLEX not explicitly contained within the tutorial.
Below is additional information important for NCLEX not explicitly contained within the tutorial.
- --
VITAL FOR NCLEX
Cardiac Ischemia: Fundamental Concepts
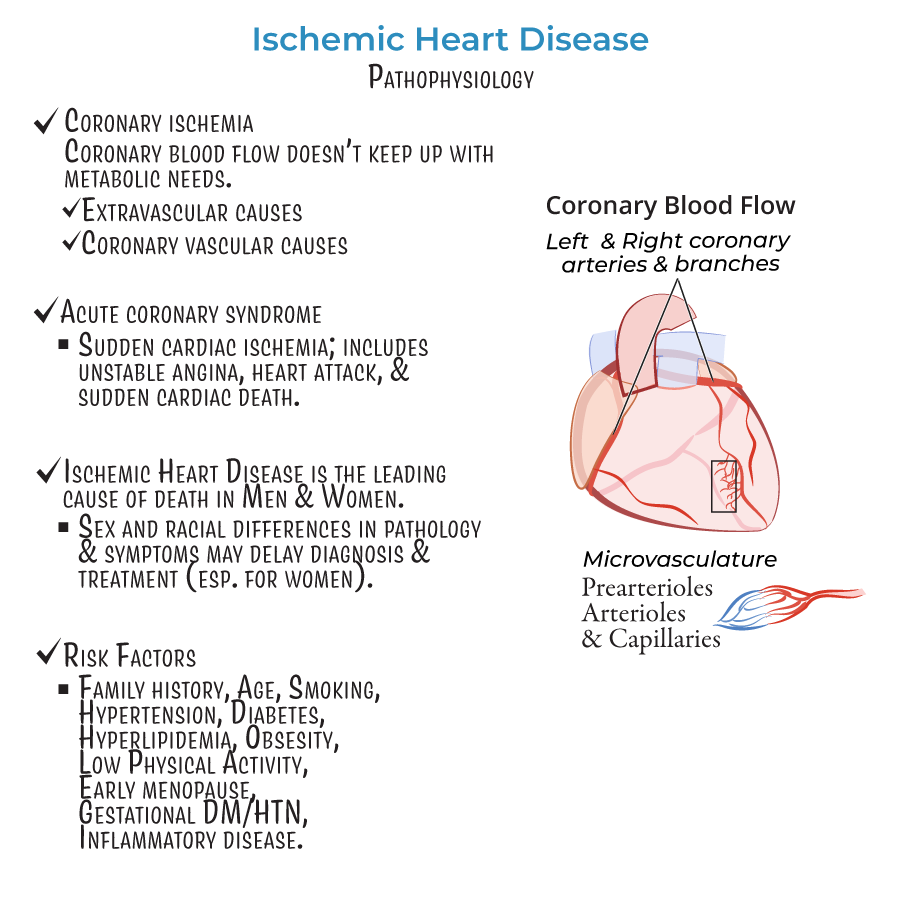
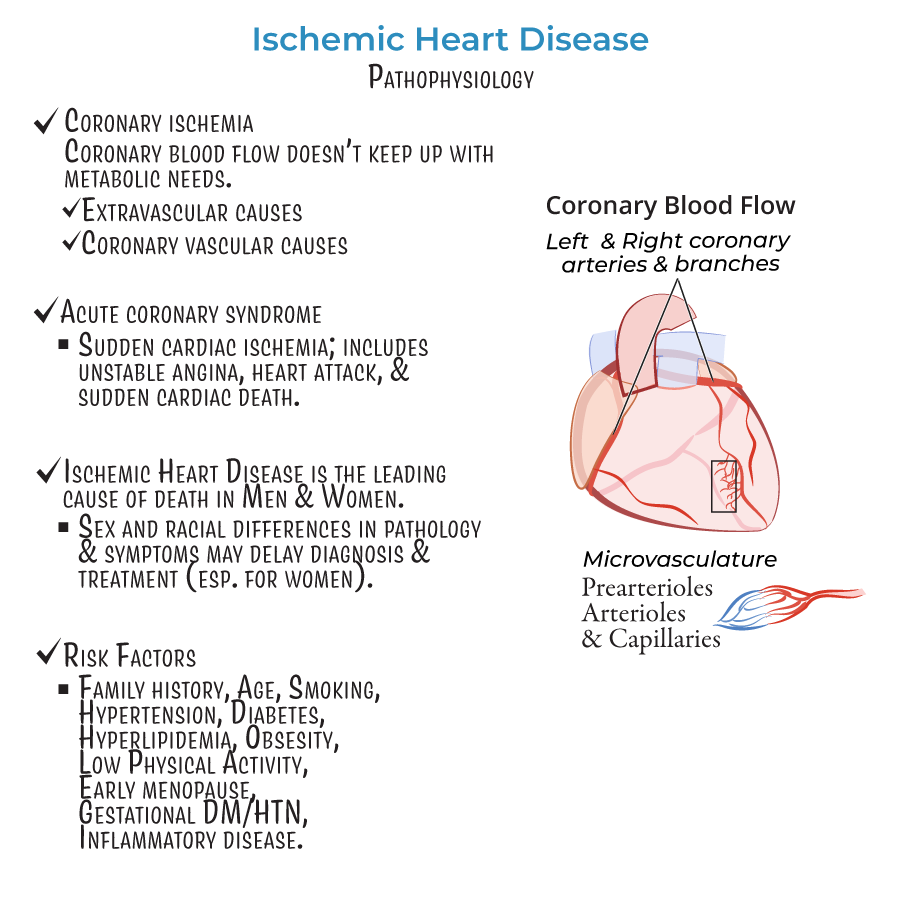
1. Definition: Cardiac ischemia occurs when coronary blood flow is insufficient to meet myocardial metabolic demands.
2. Result: Impaired mechanical and/or electrical cardiac function.
3. Patient impact: Leading cause of death in both men and women.
4. Clinical alert: Sex and racial differences may influence presentation and delay diagnosis/treatment.
Risk Factor Assessment and Screening
1. Modifiable factors: Smoking, hypertension, diabetes, hyperlipidemia, obesity, low physical activity.
2. Non-modifiable factors: Family history, age, early menopause.
3. Special considerations: Gestational diabetes/hypertension, chronic inflammatory conditions.
4. Nursing consideration: Risk factors may have stronger impacts in women than men.
Acute Coronary Syndrome Recognition
1. Definition: Umbrella term for events resulting from sudden cardiac ischemia.
2. Includes: Unstable angina, myocardial infarction, sudden cardiac death.
3. Assessment focus: Recognize symptoms that may differ between populations:
- Classic: Substernal chest pain/pressure
- Atypical: More common in women (fatigue, dyspnea, back/jaw pain)
Clinical Presentations Beyond Classic Obstruction
1. Normal angiography findings: Up to 50% of patients with suspected ischemia have no significant coronary obstruction.
2. Critical nursing insight: Normal angiogram does not exclude ischemic heart disease.
3. Alternative mechanisms to recognize:
- INOCA (Ischemia with No Obstructive Coronary Artery Disease)
- Microvascular dysfunction
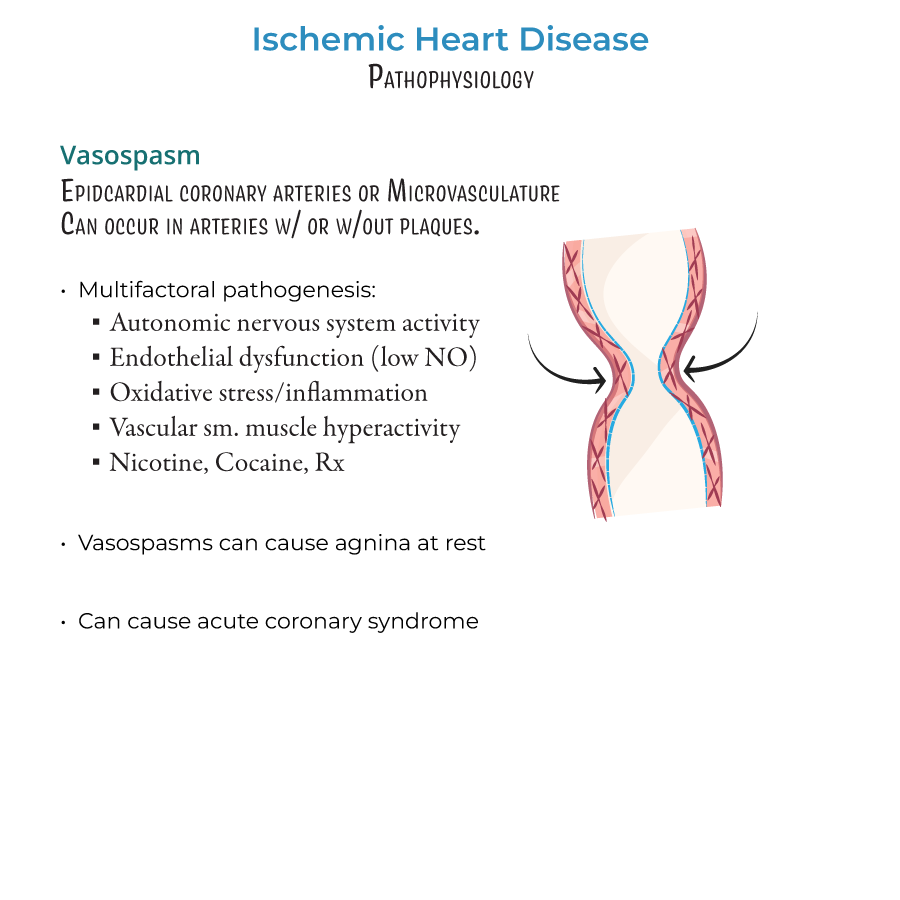
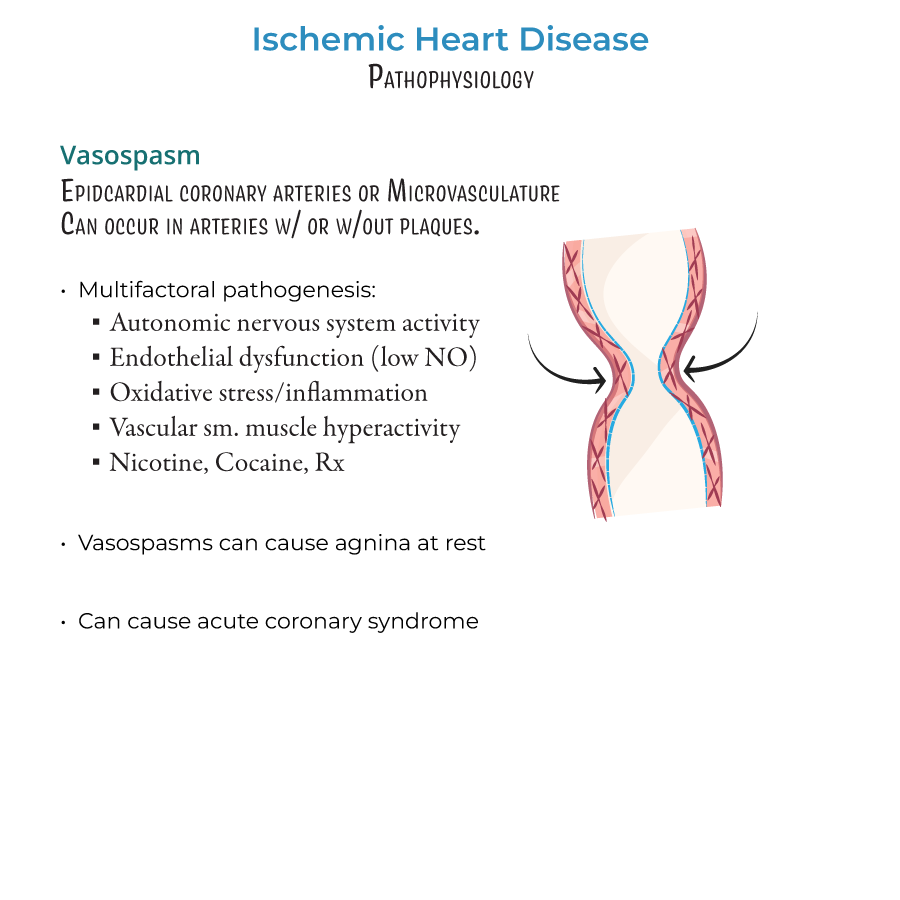
- Vasospasm
- --
HIGH YIELD
Types of Coronary Blood Supply Problems
1. Epicardial coronary arteries: Surface vessels (left and right coronary arteries and branches)
2. Coronary microvasculature: Deeper vessels (prearterioles, arterioles, capillaries)
3. Key nursing knowledge: Both large and small vessels can cause ischemia
Mechanisms of Plaque Complications
1. Plaque rupture:
- Characteristics: Lipid cores, thin caps, forms "red thrombi"
- Nursing consideration: More responsive to lipid-lowering interventions
- Patient profile: More common in women, young patients, smokers, diabetics
- Clinical significance: Increasingly important cause of acute coronary syndrome
- Nursing alert: May occur despite lipid-lowering therapy
Coronary Microvascular Dysfunction
1. Population affected: Both men and women nearly equally
2. Assessment challenge: May have normal coronary angiograms
3. Pattern of ischemia: Diffuse and patchy (vs. focal with epicardial obstruction)
4. Nursing implication: Consider in patients with continuing symptoms despite normal angiogram
Vasospasm: Nursing Considerations
1. Triggers requiring patient education:
- Autonomic nervous system activation (stress)
- Substances: nicotine, cocaine, certain medications
- Inflammatory processes
Patient-Centered Assessment Guide
1. Four mechanisms with different presentations:
- Obstructive coronary artery disease: Classic exertional symptoms
- INOCA: May have atypical presentation, especially in women
- Plaque complications: May present as acute events
- Microvascular dysfunction: Often exercise intolerance, dyspnea
- Complete cardiovascular risk assessment
- Detailed symptom evaluation (timing, triggers, relief measures)
- Recognition of atypical presentations
- Monitoring for complications of ischemia
- --
Beyond the Tutorial
Nursing Process for Ischemic Heart Disease
#
Assessment
1. History taking:
- Characteristic chest pain (PQRST assessment)
- Associated symptoms: dyspnea, diaphoresis, nausea, fatigue
- Timing of symptoms (rest vs. exertion)
- Risk factor evaluation
- Vital signs with particular attention to blood pressure and heart rate
- Heart sounds (S3, S4, murmurs)
- Respiratory assessment
- Signs of heart failure (JVD, edema, crackles)
- Perfusion status (capillary refill, extremity temperature)
- ECG changes (ST elevation/depression, T-wave inversion)
- Cardiac biomarkers (troponin, CK-MB)
- Oxygen saturation
Nursing Diagnoses
1. Acute Pain related to myocardial ischemia
2. Decreased Cardiac Output related to altered myocardial contractility
3. Activity Intolerance related to imbalance between oxygen supply and demand
4. Anxiety related to threat to health status
5. Ineffective Tissue Perfusion related to interrupted blood flow
#
Planning & Interventions
1. Acute management:
- Oxygen administration for hypoxemia (maintain O2 sat > 94%)
- Assist with administration of medications:
- Nitroglycerin: Monitor BP, headache
- Aspirin: Antiplatelet effects
- Morphine: Pain relief, anxiety reduction
- Beta-blockers: HR and BP control
- Continuous cardiac monitoring
- IV access maintenance
- Preparation for possible interventional procedures
- Activity progression based on tolerance
- Pain assessment and management
- Medication administration and side effect monitoring
- Cardiac rehabilitation coordination
- Emotional support and anxiety management
- Risk factor modification strategies
- Medication purpose, dosing, and side effects
- Recognition of warning symptoms requiring medical attention
- Lifestyle modifications (diet, exercise, stress management)
- Importance of follow-up care
Evaluation
1. Patient verbalizes pain relief
2. Vital signs within target parameters
3. No signs/symptoms of complications
4. Demonstrates understanding of discharge instructions
5. Adherence to medication regimen and lifestyle modifications
Critical Nursing Considerations
1. Medication administration:
- Nitroglycerin contraindications with PDE-5 inhibitors
- Beta-blocker cautions in certain populations
- Dual antiplatelet therapy management
- Statin administration timing and side effects
- Timely ECG for chest pain (within 10 minutes of arrival)
- Rapid triage and intervention for suspected ACS
- Continuous cardiac monitoring
- Frequent vital sign monitoring
- Coronary precautions (activity restrictions)
- Elderly: Atypical presentations, medication adjustments
- Women: Different symptom patterns, increased vigilance
- Diabetics: May have silent ischemia, complicated management
- Heart failure patients: Fluid and medication management challenges
