NCLEX - Inflammatory Bowel Disease
Start your One-Week Free Trial
Already subscribed? Log in »
Here are key facts for NCLEX from the Inflammatory Bowel Disease tutorial, as well as points of interest at the end of this document that are not directly addressed in this tutorial but should help you prepare for the boards. See the tutorial notes for further details and relevant links.
- --
VITAL FOR NCLEX
Inflammatory Bowel Disease (IBD) Overview
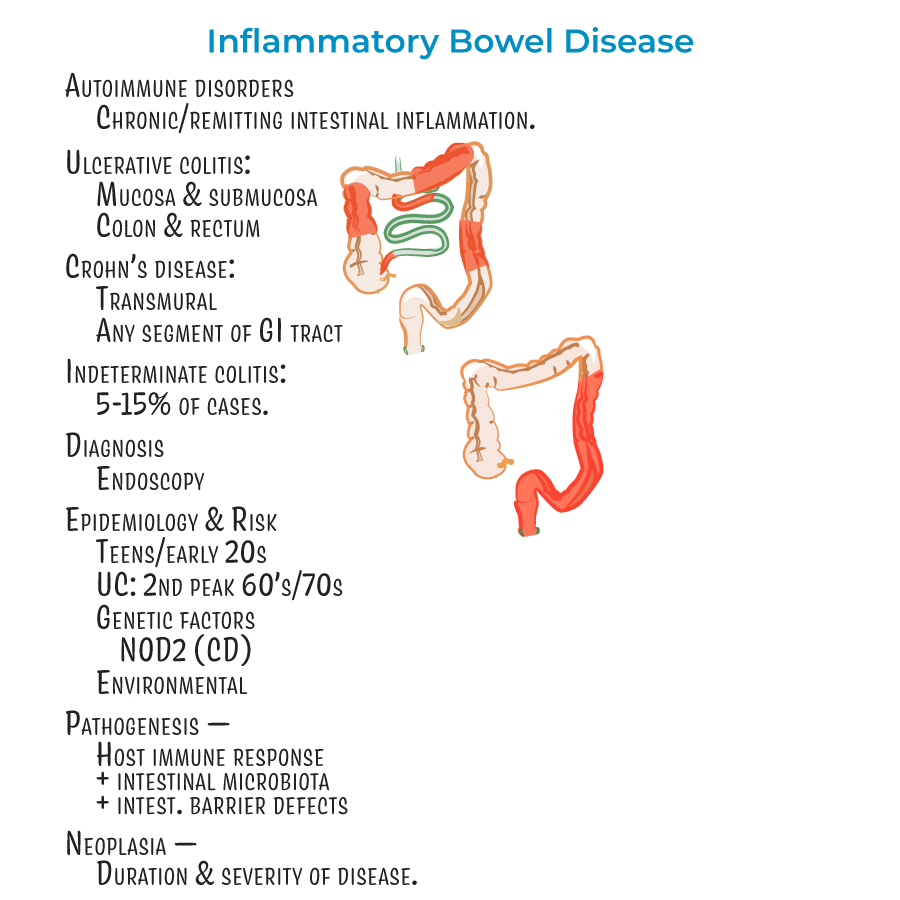
1. Autoimmune disorders characterized by chronic or remitting intestinal inflammation.
2. Diagnosis is established through endoscopy.
3. Patient demographics: Most patients diagnosed in teens/early 20s; ulcerative colitis has a second "peak" in patients in their 60's or 70's.
4. Neoplasia risk increases with duration and severity of disease - important for patient education and monitoring.
Crohn's Disease - Assessment and Care
1. Clinical presentation: Abdominal cramping (often on the right side, where the ileum meets the large intestine), diarrhea (potentially bloody), fever and malaise, weight loss (due to malabsorption), perianal lesions (25% of patients).
2. Complications to monitor for: Problems related to fistulas, fissures, and obstructive strictures; dysplasia and adenocarcinoma; and anemia from chronic blood loss.
3. Patient teaching: Advise patients to avoid cigarette smoking and nicotine as these exacerbate inflammation in Crohn's disease.
4. Distribution pattern: Can affect any segment of GI tract but most commonly involves ileum and colon with "skip lesions" (discontinuous pattern).
5. Rectum is usually spared unlike ulcerative colitis - important for differential assessment.
Ulcerative Colitis - Assessment and Care
1. Clinical presentation: Bloody diarrhea with rectal bleeding, abdominal pain, fever, and weight loss.
2. Complications requiring immediate intervention: Toxic ulceritis, toxic megacolon, intestinal perforation.
3. Patient education: Inform patients who smoke that they may experience flares upon quitting - requires careful monitoring during smoking cessation.
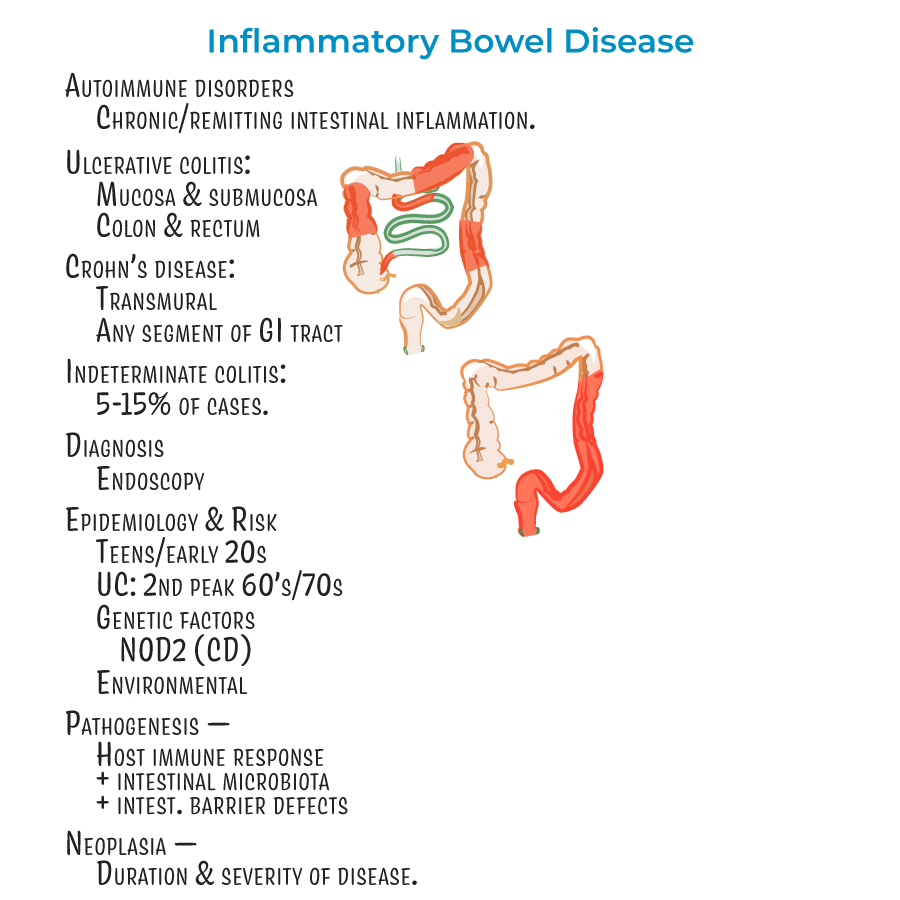
4. Distribution pattern: Restricted to the colon and rectum with continuous lesions.
5. Assessment findings: Mucosa appears bloody with friable appearance during active inflammation.
- --
HIGH YIELD
Nursing Assessment for IBD
1. Extraintestinal manifestations: Monitor for skin lesions (in up to 40% of patients), uveitis, and arthritis.
2. Assess for potentially life-threatening complications including involvement of liver/gallbladder, lung, pancreas, and kidneys.
3. Environmental factors affect management and patient education (diet, cigarette smoking, medications).
4. About 5-15% of cases are considered "indeterminant" colitis - be prepared for diagnostic uncertainty in some patients.
Crohn's Disease - Nursing Considerations
1. Gender consideration: Many studies suggest a female predominance.
2. Progressive assessment findings that indicate worsening disease:
- Aphthous erosions (early shallow whitish sores)
- Longitudinal "bear claw" ulcers (look like rake dragged down GI lining)
- Cobblestone appearance (as tissue becomes crowded with ulcers)
- Fissures and fistulas (connecting to abdominal/pelvic cavity or other organs)
Ulcerative Colitis - Nursing Considerations
1. Bleeding risk: Inflammation destroys submucosal vascular network - monitor for signs of hypovolemia and anemia.
2. Pseudopolyps may be visible on endoscopy - differentiate from precancerous lesions.
3. Colorectal cancer risk increases with disease duration, especially with pancolitis (entire colon involvement).
4. Stool assessment: Bloody diarrhea with mucus is characteristic.
5. Smoking cessation teaching: Unlike Crohn's, patients who quit smoking may experience temporary worsening of ulcerative colitis.
Treatment and Intervention Considerations
1. Medication administration and patient teaching for:
- Anti-inflammatories
- Immune suppressors
- Biologics
- Colectomy for ulcerative colitis
- Bowel resections for Crohn's disease
- --
Beyond the Tutorial
Nursing Process for IBD
#
Assessment
1. Comprehensive physical assessment:
- Abdominal assessment: tenderness, distention, masses, bowel sounds
- Perianal examination for fistulas, fissures, and skin tags
- Vital signs monitoring with attention to fever and tachycardia
- Skin assessment for extraintestinal manifestations
- Pain assessment using appropriate scale
- CBC for anemia and leukocytosis
- Inflammatory markers (ESR, CRP)
- Albumin levels for nutritional status
- Electrolyte imbalances
- Stool tests for occult blood, pathogens, and calprotectin
- Impact on activities of daily living
- Body image concerns, particularly with ostomies
- Social isolation due to bathroom urgency
- Anxiety and depression screening
- Coping mechanisms and support systems
Nursing Diagnoses
1. Diarrhea related to inflammatory process
2. Acute pain related to intestinal inflammation
3. Imbalanced nutrition: less than body requirements
4. Risk for deficient fluid volume related to diarrhea
5. Disturbed body image related to disease process or treatment
6. Anxiety related to unpredictable disease course and symptoms
7. Ineffective coping related to chronic illness
8. Risk for impaired skin integrity related to perianal complications
#
Planning and Implementation
1. Medication administration and teaching:
- Aminosalicylates (5-ASA): timing with meals, maintaining hydration
- Corticosteroids: infection risk, blood glucose monitoring, mood changes
- Immunomodulators: infection risk, regular lab monitoring, pregnancy precautions
- Biologics: administration technique, storage requirements, delayed hypersensitivity
- Antibiotics: specific timing, probiotic considerations
- Small, frequent meals during flares
- Food diary to identify triggers
- Low-fiber diet during flares; high-fiber during remission when appropriate
- Adequate protein intake for tissue healing
- Enteral or parenteral nutrition when indicated
- Stoma assessment and care
- Appliance selection and fitting
- Skin barrier protection
- Odor management
- Teaching self-care and troubleshooting
- Bowel obstruction: NPO status, NG tube management, IV fluid administration
- Toxic megacolon: frequent vital signs, abdominal assessment, positioning
- Perianal abscess: wound care, pain management, sitz baths
- Severe bleeding: hemodynamic monitoring, blood product administration
Evaluation
1. Expected outcomes:
- Reduction in frequency and severity of diarrhea
- Pain controlled to patient satisfaction
- Maintenance or improvement in nutritional status
- Absence of complications
- Effective coping with chronic illness
- Stool frequency, consistency, and presence of blood
- Weight trends and nutritional markers
- Quality of life measures
- Medication adherence and side effects
- Evidence of disease remission or progression
Patient Education and Discharge Planning
1. Medication adherence strategies:
- Visual medication schedules
- Medication reminders and organizers
- Understanding the importance of maintenance medications during remission
- Side effect management and reporting
- Symptom recognition and early intervention
- When to seek medical attention
- Stress management techniques
- Energy conservation strategies
- Bathroom mapping for travel
- Connection to support groups
- Resources for mental health services
- Strategies for managing work or school with IBD
- Intimacy and relationship counseling when needed
- Immunization recommendations with consideration for immunosuppression
- Cancer screening schedules
- Bone health with corticosteroid use
- Infection prevention strategies
- Regular follow-up appointments
- Laboratory monitoring schedule
- Endoscopic surveillance timeline
- Necessary dietary supplementation
