NCLEX - H. pylori Infection
Start your One-Week Free Trial
Already subscribed? Log in »
Here are key facts for NCLEX from the Helicobacter pylori tutorial, as well as points of interest at the end of this document that are not directly addressed in this tutorial but should help you prepare for the boards.
 Below is information not explicitly contained within the tutorial but important for NCLEX.
Below is information not explicitly contained within the tutorial but important for NCLEX.
- --
VITAL FOR NCLEX
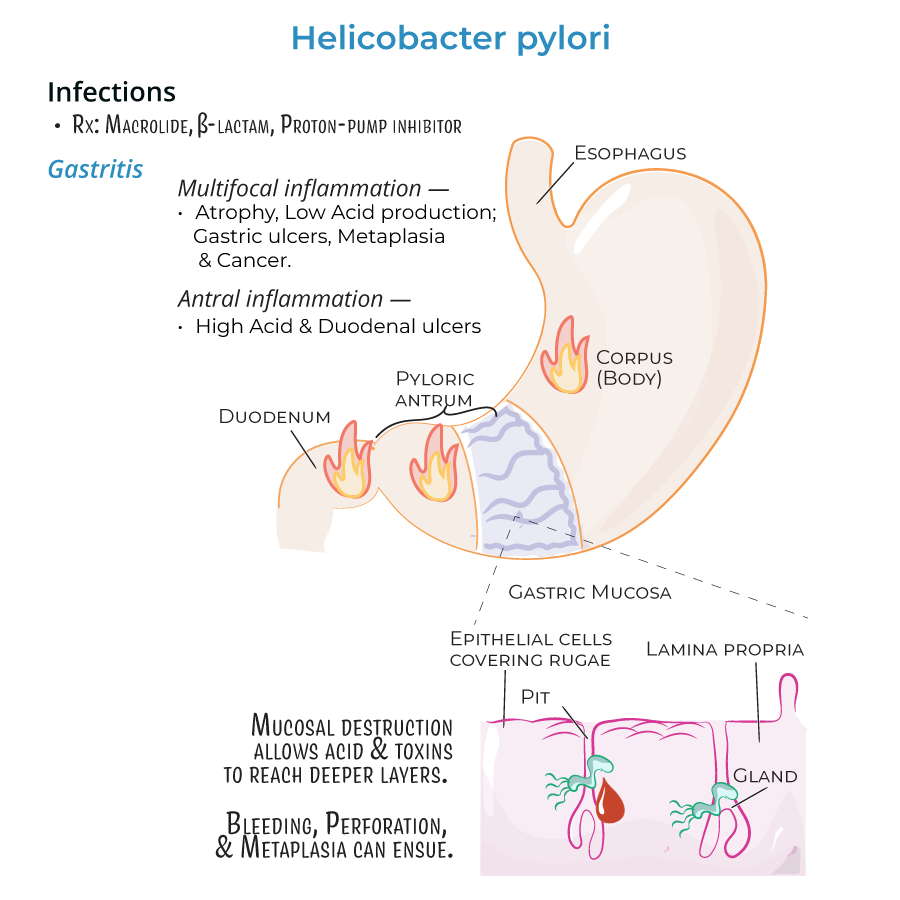
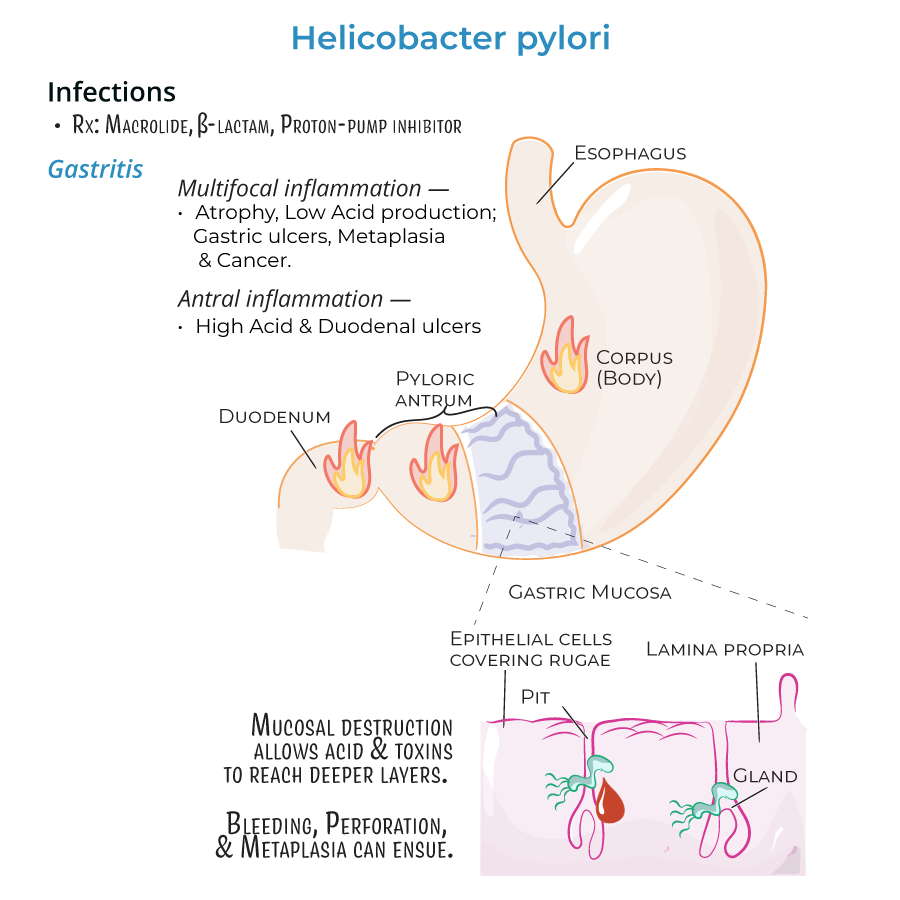
Helicobacter pylori - Assessment Findings
1. Patient history may reveal human-to-human transmission with infection typically occurring during childhood.
2. Symptoms often appear during adulthood despite life-long colonization.
3. Assessment may reveal patients are asymptomatic or experiencing nausea, bloating, and vomiting in the acute phase.
4. Patients with gastritis present with inflammation of the stomach lining.
5. Monitor for complications including peptic ulcers (10-20% of gastritis patients) and more severe conditions.
Potential Complications
1. Assess for signs of bleeding or perforation in patients with severe ulceration.
2. Monitor for development of gastric adenocarcinoma (occurs in 1-2% of chronic infections).
3. Be aware of MALT lymphoma risk when lymphoid tissues infiltrate the stomach.
4. Recognize that inflammation patterns predict different complications: antral inflammation associates with duodenal ulcers while pangastritis increases gastric cancer risk.
Treatment Administration and Patient Education
1. Administer prescribed medications including macrolides, beta-lactams, and proton-pump inhibitors.
2. Educate patients about the importance of completing full treatment course to prevent severe consequences of chronic gastritis.
3. Teach patients about medication side effects and importance of adherence to eradication therapy.
Diagnostic Testing
1. Prepare patients for tests that detect urease activity (H. pylori is urease, catalase, and oxidase positive).
2. Explain the purpose of diagnostic procedures including breath tests and endoscopy.
- --
HIGH YIELD
Detailed Assessment Parameters
1. Differentiate between localized gastritis (usually in pyloric antrum) and widespread inflammation.
2. Monitor for signs of increased or decreased acid production based on inflammation pattern.
3. Assess for neutrophil infiltration manifestations and inflammatory response.
4. Monitor for signs of bleeding, perforation, and metaplasia in patients with severe ulceration.
Risk Factors and Prevention Teaching
1. Provide education about H. pylori transmission and preventive measures.
2. Identify high-risk populations including those with family history of gastric issues.
3. Recognize that IL-8 production triggers inflammatory response with neutrophil recruitment.
4. Educate about how H. pylori destroys mucosa, allowing acids and toxins access to deeper tissues.
Medication Management
1. Explain the purpose of antibiotics in eradicating the bacterial infection.
2. Educate about proton pump inhibitors in reducing acid production and promoting healing.
3. Teach about medication interactions and timing with food.
4. Prepare patients for potential side effects of antibiotic therapy.
Special Patient Populations
1. Provide specialized care for immunocompromised patients who may develop enterohepatic helicobacter infections (H. cinaedi and H. fennelliae).
2. Recognize these related species can cause gastroenteritis and bacteremia requiring additional monitoring.
3. Implement additional precautions for patients with compromised immune systems.
4. Provide education about signs of systemic infection requiring immediate medical attention.
- --
Beyond the Tutorial
Nursing Process for H. pylori Patients
#
Assessment
1. Obtain comprehensive history including risk factors, previous treatments, and family history.
2. Assess for alarm symptoms: weight loss, dysphagia, anemia, hematemesis, melena.
3. Document medication history including NSAID use, which can exacerbate symptoms.
4. Assess nutritional status and dietary triggers that worsen symptoms.
5. Evaluate patient's understanding of the infection and treatment plan.
#
Nursing Diagnoses
1. Acute Pain related to inflammation of gastric mucosa
2. Risk for Deficient Fluid Volume related to nausea and vomiting
3. Imbalanced Nutrition: Less Than Body Requirements related to discomfort with eating
4. Deficient Knowledge related to disease process and treatment regimen
5. Risk for Ineffective Therapeutic Regimen Management related to complex medication schedule
#
Implementation
1. Administer medications as prescribed, teaching proper timing with meals.
2. Implement antiemetic measures for patients experiencing nausea.
3. Provide small, frequent meals for patients with compromised nutritional status.
4. Teach stress reduction techniques to minimize excess acid production.
5. Demonstrate how to use medication tracking tools to improve adherence.
6. Educate about foods/substances to avoid: alcohol, caffeine, spicy foods, tobacco.
#
Evaluation
1. Monitor for symptom resolution following treatment completion.
2. Assess adherence to medication regimen through patient reporting.
3. Evaluate nutritional status improvements through weight monitoring.
4. Confirm patient understanding of follow-up testing requirements.
5. Document any adverse reactions to prescribed medications.
