NCLEX - GI Bleeding
Start your One-Week Free Trial
Already subscribed? Log in »
Here are key facts for NCLEX from the GI Bleeding tutorial, as well as points of interest at the end of this document that are not directly addressed in this tutorial but should help you prepare for the boards. See the tutorial notes for further details and relevant links.
- --
VITAL FOR NCLEX
Assessment Findings
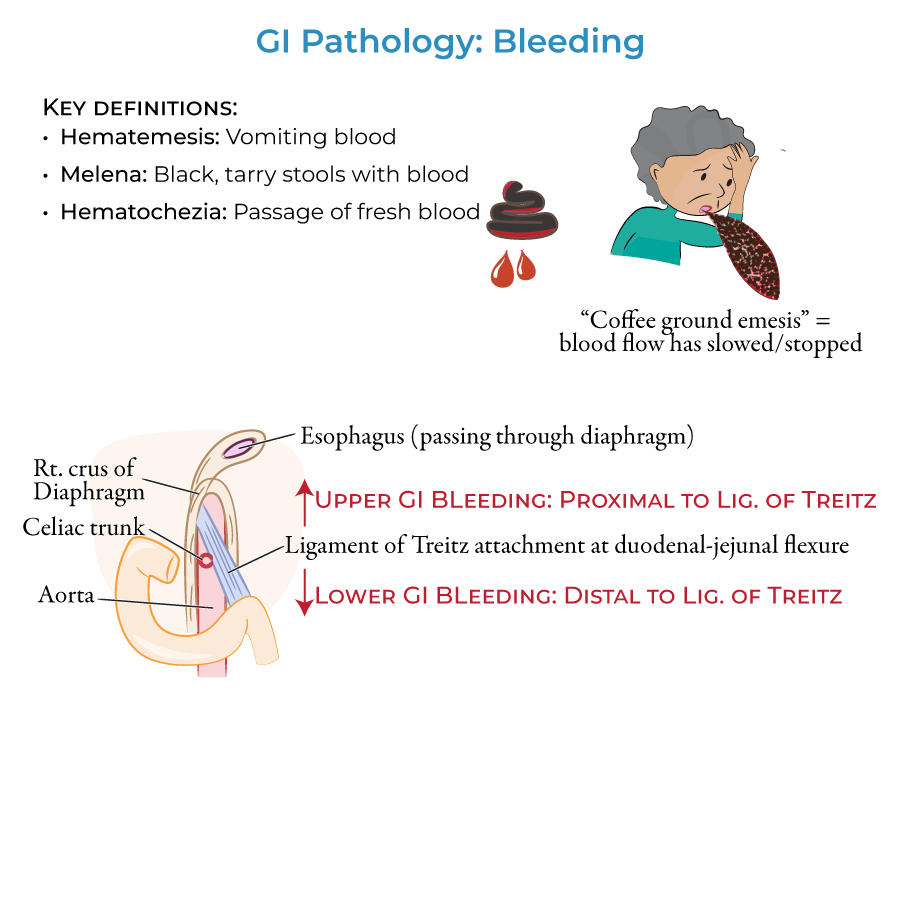
1. Hematemesis means vomiting blood ("heme" = blood; "emesis" = vomit).
2. When bloody vomit has a dark, mottled "coffee ground" appearance, this indicates that blood flow has slowed or stopped.
3. Melena refers to black, tarry stools with blood.
4. Hematochezia refers to the passage of bright red fresh blood.
5. Bleeding in the upper gastrointestinal tract produces hematemesis and/or melena; bleeding in the lower gastrointestinal tract produces melena or hematochezia.
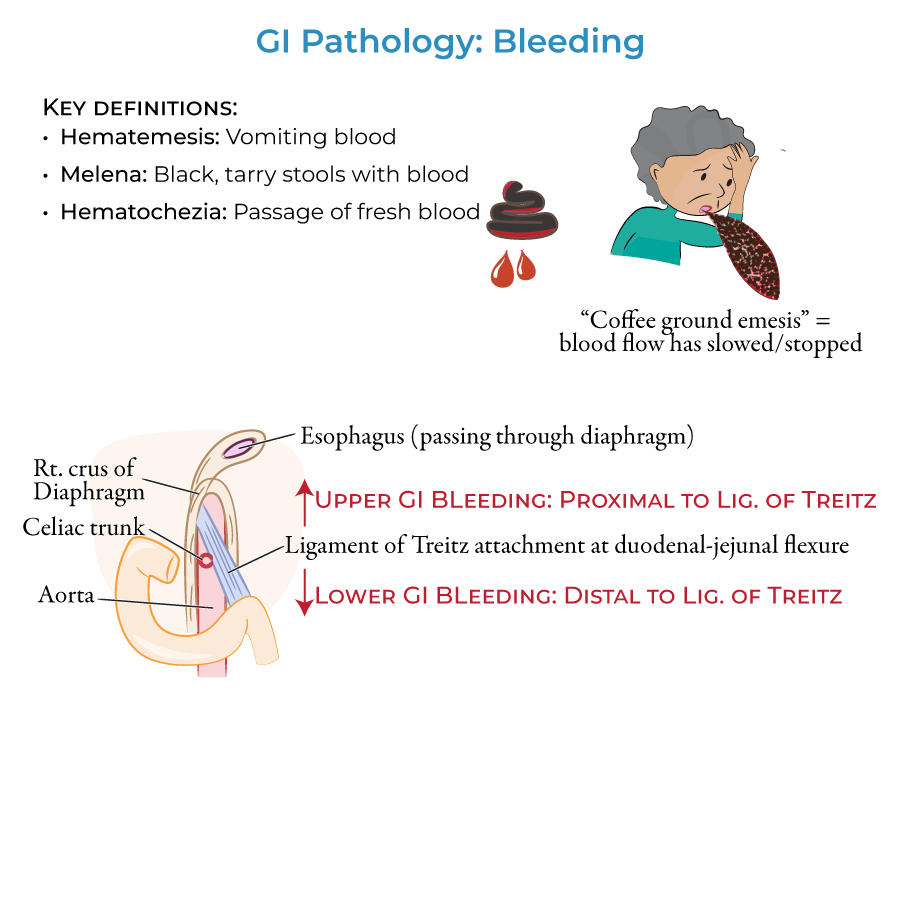
Anatomical Considerations
1. The Upper Gastrointestinal tract lies proximal to the duodenal attachment of the ligament of Treitz (suspensory ligament of the duodenum) and the Lower Gastrointestinal tract lies distal to it.
Priority Upper GI Bleeding Conditions
1. Duodenal and gastric ulcers & erosion are most common causes of upper GI bleeding, resulting from H. pylori infection, drugs, stress, or autoimmune disorders.
2. Esophagitis leads to erosion of the esophageal lining and bleeding, associated with severe acid reflux and alcohol consumption.
3. Varices in the esophagus and proximal stomach can rupture and cause potentially life-threatening hemorrhages, associated with cirrhosis and portal hypertension.
4. Mallory-Weiss tears occur in the distal esophagus from fits of violent vomiting or coughing.
Priority Lower GI Bleeding Conditions
1. Infectious colitis, particularly bacterial, produces fever, tenesmus, abdominal pain, and purulent, loose bloody stools.
2. C. difficile infection following antibiotic use is an important cause of bacterial colitis.
3. Inflammatory bowel disease, particularly ulcerative colitis, causes bloody diarrhea when active.
4. Diverticular hemorrhage is a top cause of lower GI bleeding with brisk hematochezia and potential for massive bleeding.
5. Hemorrhoids are swollen veins in the rectum and perianal region that can rupture and produce hematochezia.
- --
HIGH YIELD
Assessment Distinctions
1. "Coffee ground" appearance of vomit indicates that blood flow has slowed or stopped.
2. Viral colitis is associated with watery diarrhea and is more common in infants and children.
3. Amoebic colitis is associated with diarrhea and mucoid discharge.
4. Anal fissures produce bright, fresh blood and cause pain during and after bowel movements.
5. Acute and chronic intestinal ischemia causes lower GI bleeding along with nausea, vomiting, and abdominal pain.
Patient Monitoring Considerations
1. Varices can cause potentially life-threatening hemorrhages and require vigilant monitoring.
2. Ulcerative colitis is characterized by mucosal and submucosal inflammation with sunken ulcers creating a friable or crumbly appearance.
3. Diverticula are not necessarily inflamed when bleeding occurs in diverticular hemorrhage.
4. Mallory-Weiss tears are rare compared to other causes of upper GI bleeding.
5. Neoplasms can occur anywhere along the GI tract and are often the presenting sign.
Additional Clinical Considerations
1. Arteriovenous malformations are atypical arrangements of blood vessels that can rupture and cause bleeding. These are rare.
2. Esophagitis erosion is most often associated with severe acid reflux and alcohol consumption.
- --
Beyond the Tutorial
Nursing Assessment
1. Monitor vital signs frequently with focus on signs of hypovolemia (tachycardia, hypotension, decreased urine output).
2. Assess and document all gastric output and stool characteristics (color, amount, frequency).
3. Implement abdominal assessment, noting distention, tenderness, and bowel sounds.
4. Calculate fluid balance by measuring all intake and output.
5. Evaluate laboratory values including hemoglobin, hematocrit, BUN/creatinine ratio, and coagulation studies.
Nursing Interventions
1. Position patients with active bleeding in left lateral position to prevent aspiration.
2. Administer IV fluids and blood products as ordered to maintain hemodynamic stability.
3. Insert and maintain nasogastric tubes for patients with upper GI bleeding.
4. Prepare patients for diagnostic procedures including endoscopy and colonoscopy.
5. Administer medications as prescribed (PPIs, octreotide, antibiotics for C. difficile).
Patient Education
1. Teach patients to recognize and report signs of GI bleeding promptly.
2. Provide education on medication adherence for H. pylori eradication.
3. Instruct patients with varices about avoiding activities that increase portal pressure.
4. Educate patients with inflammatory bowel disease about dietary modifications and medication regimens.
5. Teach patients with hemorrhoids about proper hygiene and dietary fiber intake.
Nursing Priorities
1. Recognize early signs of shock and implement appropriate interventions.
2. Maintain airway patency in patients with massive hematemesis.
3. Implement fall precautions for patients with anemia secondary to blood loss.
4. Provide emotional support to patients experiencing acute GI bleeding.
5. Facilitate communication between healthcare team members regarding patient status changes.
