NCLEX - Gastritis & Peptic Ulcer Disease
Start your One-Week Free Trial
Already subscribed? Log in »
Here are key facts for NCLEX from the Gastritis & Peptic Ulcer Disease tutorial, as well as points of interest at the end of this document that are not directly addressed in this tutorial but should help you prepare for the boards. See the tutorial notes for further details and relevant links.
 Below is information not explicitly contained within the tutorial but important for NCLEX-RN.
Below is information not explicitly contained within the tutorial but important for NCLEX-RN.
- --
VITAL FOR NCLEX-RN
Assessment & Clinical Manifestations
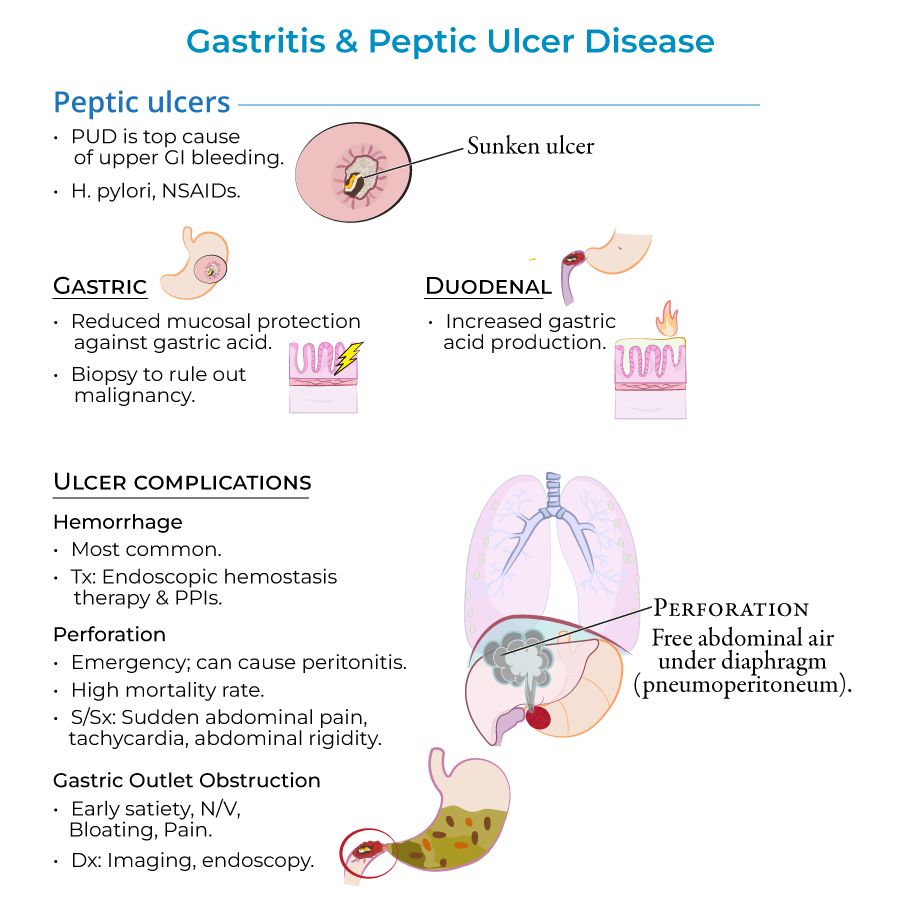
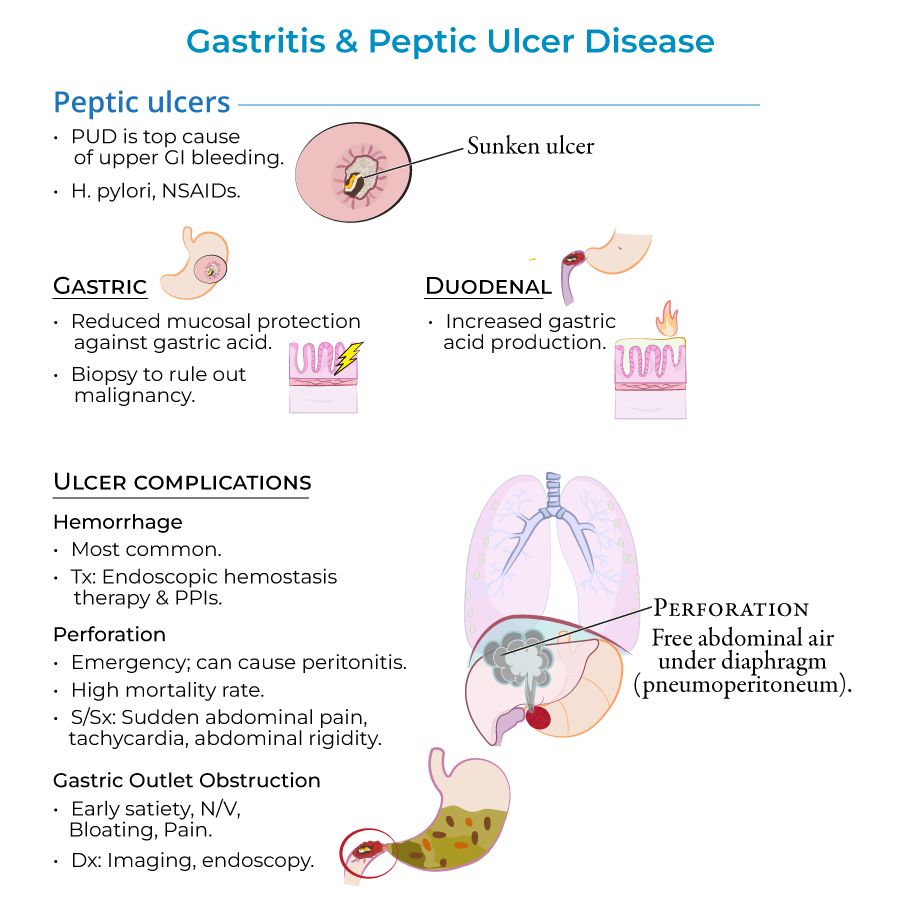
1. Signs and symptoms include epigastric pain, GI bleeding, nausea or vomiting; many patients are asymptomatic, especially in early phases.
2. Gastric ulcer pain increases upon eating, leading patients to avoid food and lose weight.
3. Duodenal ulcer pain relieves with eating and may be associated with weight gain, though these patterns are not always consistent.
4. Perforation presents with sudden abdominal pain, tachycardia, and abdominal rigidity - requires immediate intervention.
5. Gastric outlet obstruction manifests with early satiety, nausea, vomiting, bloating, and pain.
Diagnostic Tests & Monitoring
1. Diagnosis relies on upper endoscopy to visualize lesions and biopsies to assess inflammation, H. pylori infection, and malignancy.
2. Urea breath test and stool antigen tests are non-invasive methods for detecting active H. pylori infection.
3. H. pylori antibody serologies do not distinguish between active and inactive disease - not useful for confirming active infection.
4. For patients older than 60 years or with alarming symptoms (weight loss, anemia, bloody stools, dysphagia), upper endoscopy should be performed.
5. Follow-up testing is necessary to confirm H. pylori eradication and prevent relapse.
Nursing Interventions & Medications
1. Treatment involves proton pump inhibitors, NSAID discontinuation, and H. pylori eradication with antibiotics when present.
2. Hemorrhagic bleeding can be deadly, requiring prompt treatment with proton pump inhibitors and close monitoring.
3. For gastric outlet obstruction, treatment of the underlying peptic ulcer disease is attempted before surgical solutions.
4. Stress ulcers require preventive care in high-risk patients with systemic burns (Curling ulcers) or brain injury (Cushing ulcers).
5. Non-ulcer dyspepsia is treated with proton pump inhibitors after ruling out cancer in those over 55 years old.
- --
HIGH YIELD
Risk Factors & Prevention
1. H. pylori is present in 70% of gastric ulcer cases and 90% of duodenal ulcers - a key modifiable risk factor.
2. NSAIDs, aspirin, and alcohol are common causes of acute gastritis, especially when alcohol and aspirin are combined.
3. NSAIDs block prostaglandin synthesis necessary for mucous production, while alcohol causes direct damage to the mucosal lining.
4. Cigarette smoking is an important risk factor for peptic ulcer disease that should be addressed in patient education.
5. Contrary to popular belief, psychological stress and spicy foods do not cause peptic ulcers - important for patient education.
Complications & Priority Assessments
1. Peptic ulcers are the most common cause of upper GI bleeding, though most ulcers do not bleed.
2. Perforation has a high mortality rate (up to 30%) - monitor for sudden abdominal pain, tachycardia, and abdominal rigidity.
3. Imaging of perforation will show free abdominal air under the diaphragm (pneumoperitoneum).
4. Gastric ulcers have a higher risk of malignancy (5-10%) compared to duodenal ulcers, making early detection crucial.
5. Chronic inflammation from either disorder can pave the way for malignancy, requiring vigilant follow-up care.
Special Populations & Considerations
1. Autoimmune gastritis involves destruction of parietal cells and can lead to pernicious anemia requiring B12 monitoring.
2. Patients with autoimmune gastritis are likely to have other autoimmune disorders requiring comprehensive care.
3. Cases of NSAID-related peptic ulcers are increasing, possibly due to an aging population relying on NSAIDs for pain relief.
4. For patients younger than 60 years without alarming symptoms, focus on non-invasive H. pylori testing and PPI response.
5. Curling ulcers develop when systemic burns cause hypovolemia and mucosal ischemia, while Cushing ulcers develop from brain injury with increased vagal stimulation.
- --
Beyond the Tutorial
Nursing Care Plan Priorities
1. Pain management: Assess pain characteristics (timing, location, aggravating/alleviating factors) to differentiate between gastric and duodenal ulcers.
2. Nutritional assessment: Monitor weight, intake/output, and dietary patterns; implement small, frequent meals for patients with gastric outlet obstruction.
3. Medication teaching: Educate patients about proper administration of PPIs (before meals), antibiotic regimens for H. pylori, and NSAID alternatives.
4. Bleeding precautions: Monitor for melena, hematemesis, dizziness, and orthostatic hypotension; check hemoglobin/hematocrit levels regularly.
5. Discharge planning: Provide education on smoking cessation, dietary modifications, stress management techniques, and medication adherence.
Critical Nursing Interventions
1. Emergency response to perforation: Position patient for comfort, maintain NPO status, prepare for immediate surgical intervention, and monitor vital signs.
2. GI bleeding management: Administer IV fluids as ordered, monitor for shock symptoms, prepare for possible endoscopic intervention or blood transfusion.
3. Medication administration: Space antibiotics appropriately to maximize effectiveness for H. pylori eradication.
4. Patient education: Emphasize importance of completing full antibiotic course for H. pylori, even if symptoms resolve quickly.
5. Psychosocial support: Address anxiety and misconceptions about disease cause and prognosis to improve adherence to treatment plan.
