NCLEX - Endocarditis
Start your One-Week Free Trial
Already subscribed? Log in »
Here are key facts for NCLEX from the Endocarditis tutorial, as well as points of interest at the end of this document that are not directly addressed in this tutorial but should help you prepare for the boards. See the tutorial notes for further details and relevant links.
 Additional information important for NCLEX:
Additional information important for NCLEX:
- --
VITAL FOR NCLEX
Definition and Assessment
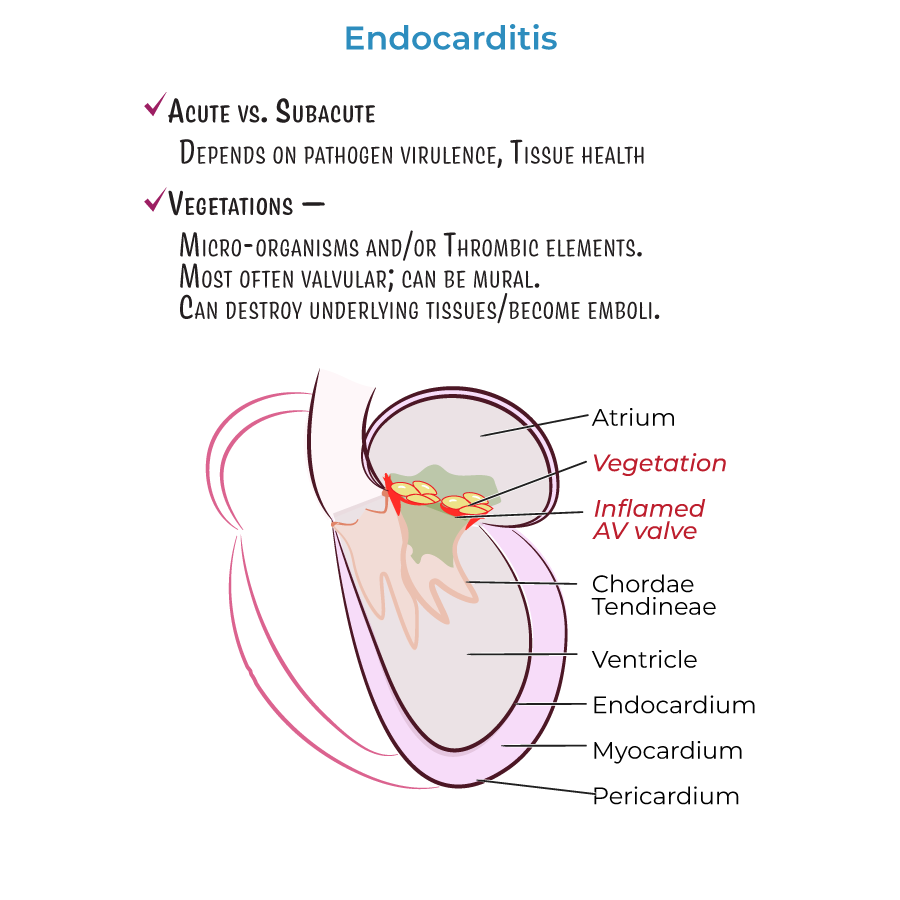
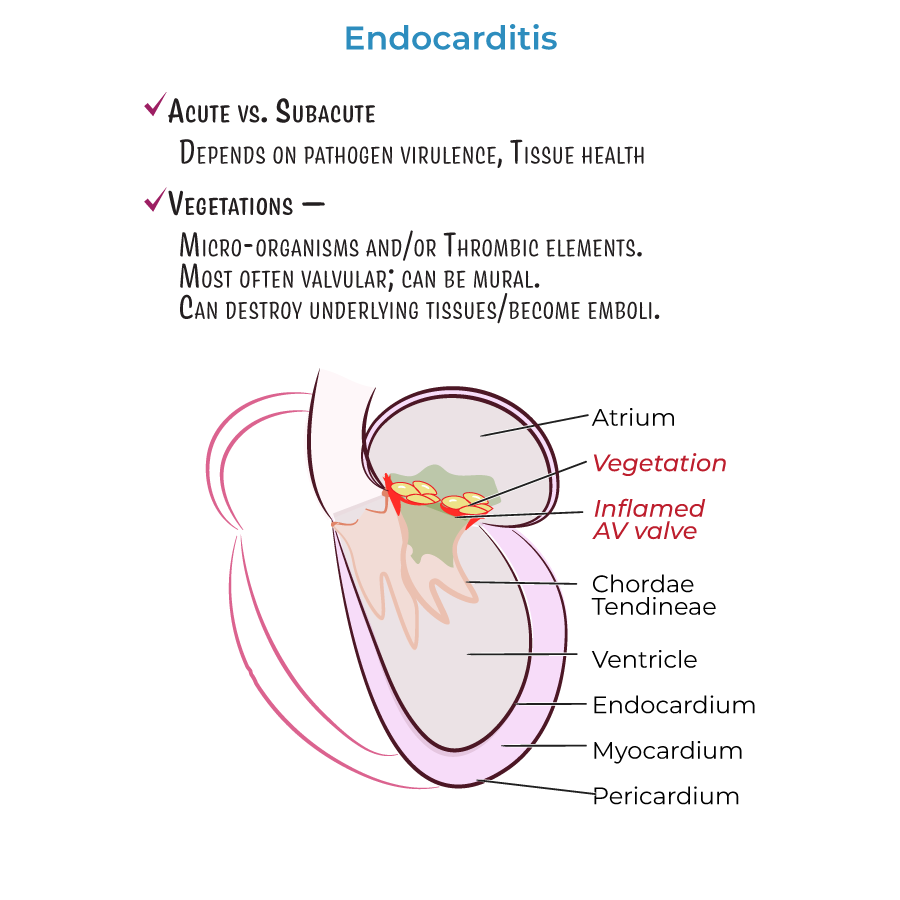
1. Endocarditis = inflammation of the internal lining of the heart (endocardium).
2. Acute endocarditis presents with fever, chills, and other flu-like symptoms.
3. Characterized by formation of vegetations comprising microorganisms and/or thrombotic elements.
4. Vegetations can invade and destroy underlying tissues or break free and become emboli.
5. Complications include stroke, organ failure, and sepsis when emboli lodge in blood vessels.
Risk Factor Assessment
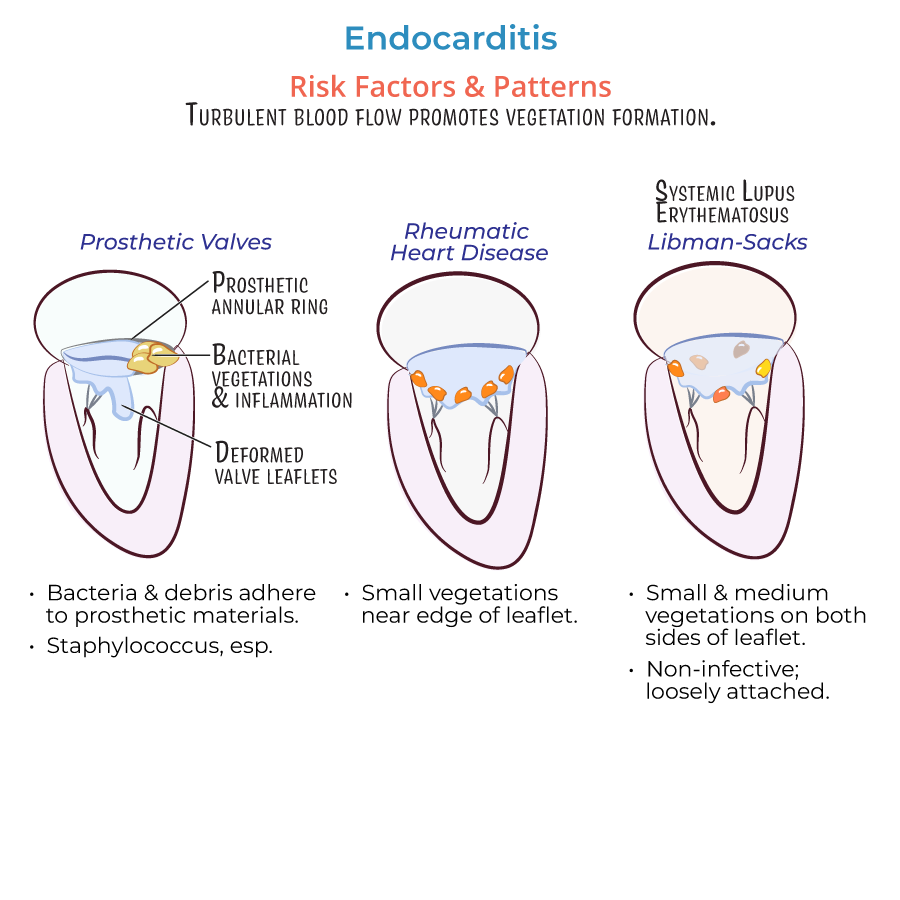
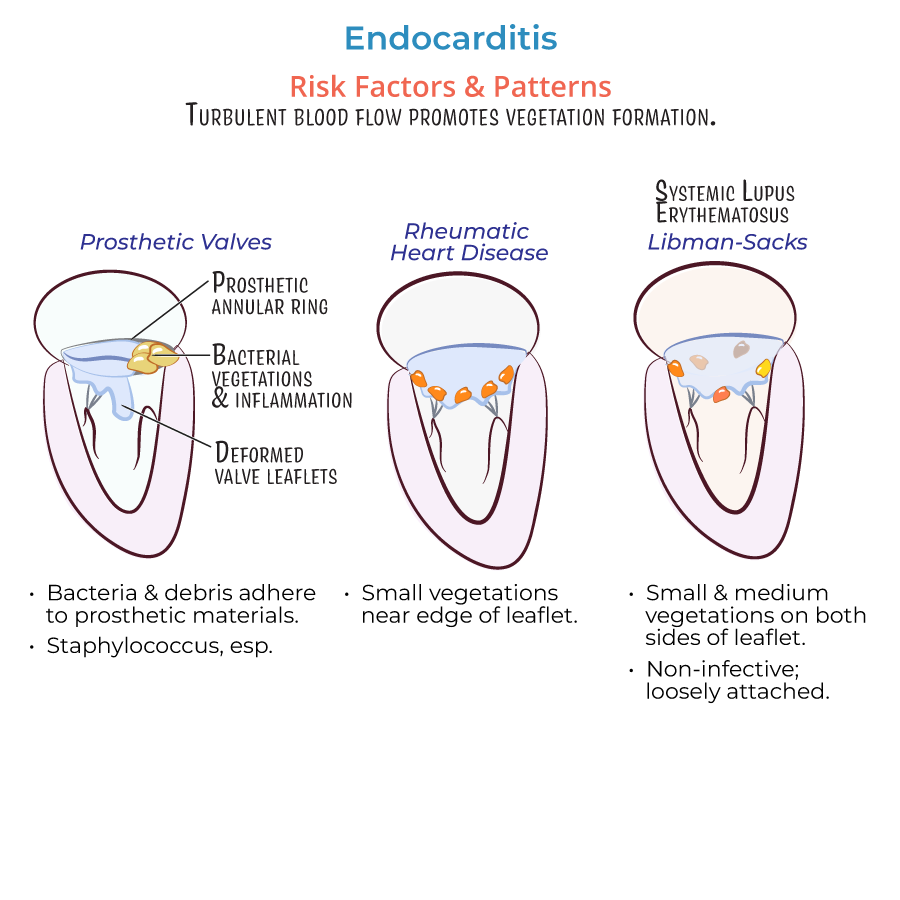
1. Valvular damage: Increases likelihood of vegetation formation.
2. Intravenous drug use: Major cause of right-sided valvular endocarditis due to:
- Particulate matter (talc) introduction
- Surface pathogens from skin
- Oral bacterial flora (if saliva used on injection needles)
- Bacteria and debris adherence to prosthetic materials
- Vulnerable environment during surgery/healing process
Types of Endocarditis for Patient Care
1. Infective endocarditis: Contains pathogens in vegetations
- Most commonly caused by gram-positive bacteria (Staphylococcus aureus, Viridans streptococci)
- Libman-Sacks endocarditis associated with Systemic Lupus Erythematosus
- --
HIGH YIELD
Clinical Manifestations and Monitoring
1. Vegetation formation process:
- Endothelial damage promotes fibronectin deposition
- Fibronectin adheres to circulating fibrin, platelets, white blood cells, and pathogens
- Vegetations can break free causing embolism or pathogen spread
Patient-Specific Considerations
1. Valve-specific manifestations:
- Mitral valve regurgitation: Produces lesions on atrial leaflet surface
- Aortic insufficiency: Produces vegetations on ventricular side
- Ventricular septal defects: Right-sided vegetations near the orifice
- Rheumatic heart disease: Small vegetations near edge of leaflet
- Libman-Sacks endocarditis (SLE):
- Small/medium vegetations on both sides of leaflets
- Loosely attached with increased embolism risk
- Invasive vegetations form where prosthetic annular ring meets tissue
- Can deform valvular leaflets
- Often requires surgical valve replacement
Pathogen-Specific Considerations
1. Common bacterial pathogens:
- Gram-positive: Staphylococcus aureus, Viridans streptococci, Enterococci, Coagulase-negative staphylococci
- HACEK group: Haemophilus, Aggregatibacter, Cardiobacterium, Eikenella, Kingella
- --
Beyond the Tutorial
Nursing Assessment
1. Cardinal signs: Fever, new or changed heart murmur, embolic phenomena
2. Physical assessment findings:
- Janeway lesions: Painless, erythematous macules on palms/soles
- Osler nodes: Painful, tender nodules on fingers/toes
- Splinter hemorrhages: Linear dark streaks under nails
- Roth spots: Retinal hemorrhages with pale centers
Nursing Interventions
1. Monitoring:
- Vital signs with focus on temperature patterns and cardiac assessment
- Signs of embolic events (neurological changes, abdominal pain, hematuria)
- Blood cultures before antibiotic administration
- IV antibiotics administration (often for 4-6 weeks)
- Monitoring for adverse effects of long-term antibiotic therapy
- Activity monitoring and progressive ambulation
- Heart failure assessment and management
- Infection control practices
Patient Education
1. Antibiotic compliance: Importance of completing full course
2. Signs of complications: When to seek immediate medical attention
3. Endocarditis prophylaxis: For high-risk patients undergoing dental/invasive procedures
4. IV drug users: Resources for addiction treatment and harm reduction
5. Follow-up care: Importance of follow-up echocardiograms and appointments
