NCLEX - ECG
Start your One-Week Free Trial
Already subscribed? Log in »
Here are key facts for NCLEX (National Council Licensure Examination) from the Electrocardiogram/ECG, EKG tutorial, focusing on the nursing process, patient care, and clinical judgment essential for licensure. See the tutorial notes for further details and relevant links.
 3. Nursing Role in ECG Acquisition:
Below is information not explicitly contained within the tutorial but important for NCLEX preparation.
3. Nursing Role in ECG Acquisition:
Below is information not explicitly contained within the tutorial but important for NCLEX preparation.
- --
VITAL FOR NCLEX
Basic ECG Principles & Nursing Responsibilities
1. ECG Fundamentals:
- ECG reflects and records electrical activity of the heart muscle
- Movement of action potentials through cardiac muscle produces extracellular signals detected by ECG
- Normal resting potential of ventricular cardiac cells is approximately -90 millivolts
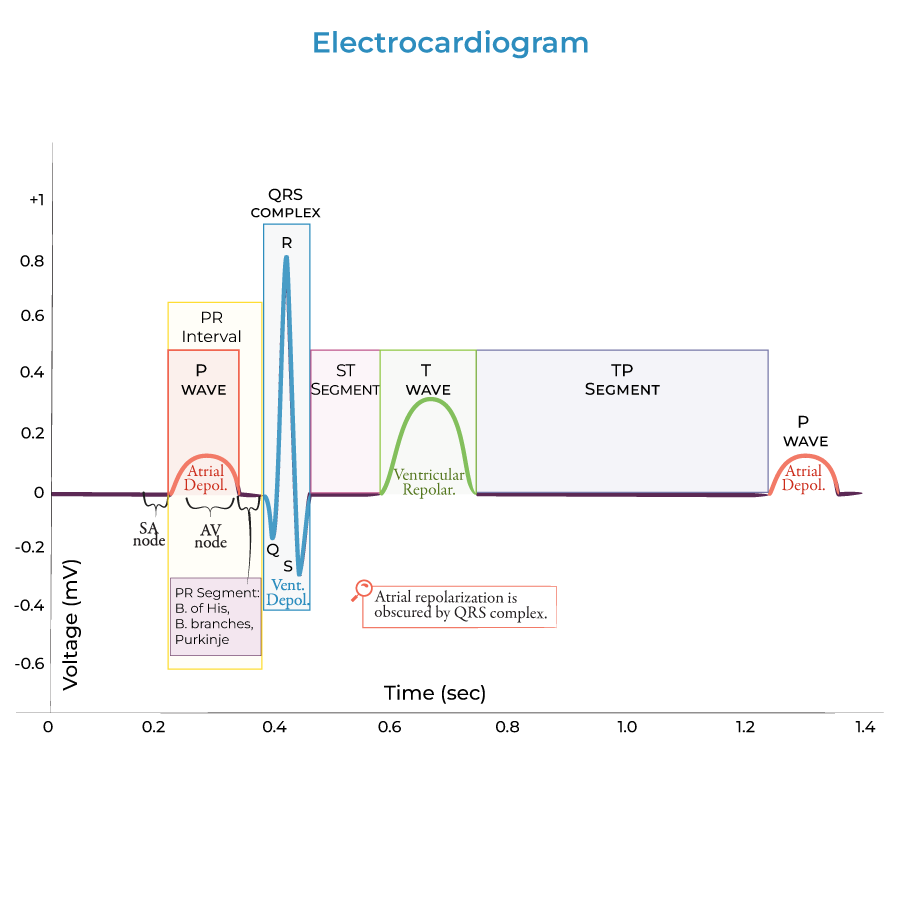
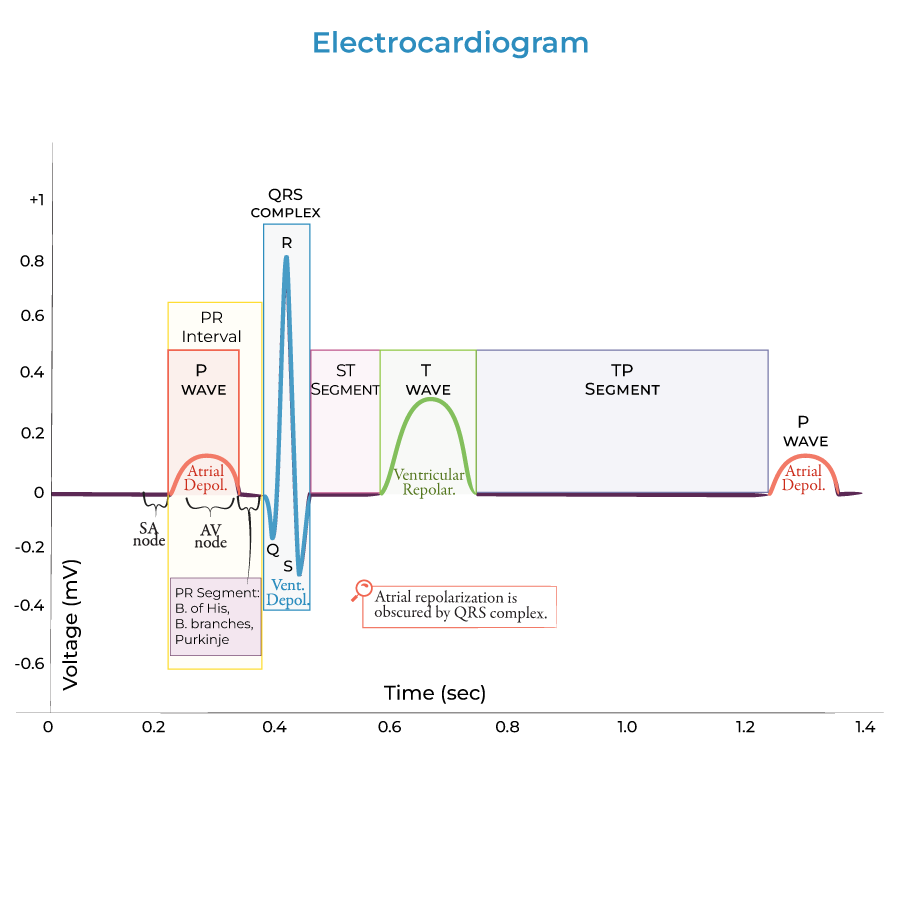
- Waves: P wave (atrial depolarization), QRS complex (ventricular depolarization), T wave (ventricular repolarization)
- Segments: Represent time spent at baseline between waves
- Intervals: Include both segments and waves (PR, QRS, QT)
 3. Nursing Role in ECG Acquisition:
3. Nursing Role in ECG Acquisition:
- Proper electrode placement
- Reducing artifact through patient positioning and education
- Documentation of patient symptoms during recording
- Recognition of normal sinus rhythm
- Identification of basic rhythm changes requiring notification
- Correlation of rhythm changes with patient assessment findings
Normal ECG Characteristics & Assessment
1. Normal Parameters:
- Heart rate: 60-100 beats per minute
- PR interval: 0.12-0.20 seconds
- QRS duration: Less than 0.12 seconds
- Sinoatrial (SA) node → atria → AV node → bundle of His → bundle branches → Purkinje fibers
- Functional significance: Ensures coordinated contraction from apex to base
- P wave: Small positive deflection
- QRS complex: Rapid, tall deflection
- T wave: Wider and taller than P wave
- U wave: Occasionally present after T wave
- Regularity of rhythm
- Presence of P wave before each QRS complex
- Consistent PR interval
- --
Beyond the Tutorial
ECG Monitoring & Telemetry Nursing Care
1. Equipment Management:
- Proper lead placement for accurate waveform acquisition
- Troubleshooting common technical issues (artifact, lead disconnect)
- Electrode site care to prevent skin breakdown
- Appropriate alarm parameter settings
- Response to alarms and documentation
- Frequency of rhythm strip documentation
- Optimal positions for clear signal acquisition
- Activity restrictions based on monitoring needs
- Managing monitoring during patient transport
- Rhythm interpretation and changes
- Correlation with patient symptoms
- Interventions and patient response
- Explaining purpose and duration of monitoring
- Addressing concerns about continuous observation
- Teaching about activity limitations with monitoring equipment
Common Arrhythmia Recognition & Nursing Interventions
1. Sinus Node Abnormalities:
- Sinus tachycardia: Rate >100 bpm, normal P waves
- Sinus bradycardia: Rate <60 bpm, normal P waves
- Sinus arrhythmia: Variation with respiratory cycle
- Atrial fibrillation: Irregular rhythm, absence of distinct P waves
- Atrial flutter: Regular "saw-tooth" pattern
- Premature atrial contractions: Early P wave with normal QRS
- Premature ventricular contractions: Wide, bizarre QRS without preceding P wave
- Ventricular tachycardia: Rapid, wide QRS complexes
- Ventricular fibrillation: Chaotic, irregular waveforms
- First-degree AV block: Prolonged PR interval
- Second-degree AV block: Intermittently dropped QRS
- Third-degree AV block: P waves and QRS complexes without relationship
- Immediate actions for life-threatening arrhythmias
- Assessment of hemodynamic stability with each arrhythmia
- Preparation of emergency equipment and medications
Electrolyte Imbalances & ECG Findings
1. Potassium Abnormalities:
- Hyperkalemia: Tall, peaked T waves progressing to widened QRS
- Hypokalemia: Flattened T waves, prominent U waves, ST depression
- Hypercalcemia: Shortened QT interval
- Hypocalcemia: Prolonged QT interval
- Hypomagnesemia associated with arrhythmias, especially in conjunction with other electrolyte imbalances
- Recognition of ECG changes suggesting electrolyte disturbances
- Correlation with laboratory values
- Monitoring during electrolyte replacement
- Safe administration of electrolyte replacements
- Monitoring for resolution of ECG changes
- Patient education regarding electrolyte balance
ECG Changes in Cardiac Emergencies
1. Myocardial Ischemia and Infarction:
- ST segment elevation or depression
- T wave inversions
- Development of Q waves
- Immediate assessment and intervention
- Oxygen administration and positioning
- Preparation for medication administration
- Low voltage QRS complexes
- Electrical alternans (alternating QRS amplitude)
- Sinus tachycardia most common
- Right heart strain patterns in severe cases
- Recognizing ECG changes requiring immediate intervention
- Preparation for emergent procedures
- Ongoing monitoring during treatment
Medication Effects on ECG & Nursing Considerations
1. Antiarrhythmic Medications:
- Beta blockers: Heart rate reduction, PR prolongation
- Calcium channel blockers: PR prolongation, AV block
- Class III antiarrhythmics: QT prolongation requiring careful monitoring
- Digoxin effect: "Scooped" ST segments, shortened QT
- Toxicity monitoring: Arrhythmias, conduction blocks
- Identification of common QT-prolonging drugs
- Monitoring protocol for patients on these medications
- Pre- and post-medication ECG monitoring
- Recognition of therapeutic vs. toxic effects
- Appropriate timing of medication administration
- Teaching about medication effects and side effects
- Signs and symptoms requiring medical attention
- Importance of adherence and follow-up monitoring
Clinical Correlation & Patient Assessment
1. Integration with Vital Signs:
- Correlation between ECG findings and blood pressure, pulse, respiration
- Recognizing discrepancies between ECG and palpated pulse (pulse deficit)
- Tachycardia (>100 bpm) and bradycardia (<60 bpm)
- Basic rhythm irregularities
- Wide QRS complexes indicating conduction delays
- Chest pain or discomfort
- Palpitations or irregular heartbeat sensation
- Dizziness, lightheadedness, or syncope
- Shortness of breath
- Rhythm characteristics
- Patient symptoms during monitoring
- Interventions performed and response
Nursing Interventions for ECG Abnormalities
1. Basic Response to Arrhythmias:
- Assessment of patient stability (ABCs)
- Oxygen administration per protocol
- Positioning for comfort and optimal cardiac output
- Notification of healthcare provider
- Continuous vs. intermittent monitoring based on clinical condition
- Evaluation of telemetry alarms and appropriate settings
- Documentation of rhythm changes and associated symptoms
- Common cardiac medications and expected ECG effects
- Monitoring for therapeutic and adverse effects on ECG
- Appropriate timing of pre- and post-medication ECGs
- Cardioversion preparation and care
- Temporary pacing assistance
- Post-procedure monitoring requirements
Patient Education & Discharge Planning
1. Disease Process Education:
- Basic explanation of cardiac conduction system
- Relationship between symptoms and cardiac rhythm
- Importance of follow-up monitoring
- Purpose of cardiac medications
- Signs of adverse effects requiring medical attention
- Importance of adherence to prescribed regimen
- Pulse checking technique
- Symptoms requiring medical attention
- Use of home monitoring devices if prescribed
- Activity recommendations based on cardiac status
- Stress reduction techniques
- Dietary considerations for cardiac health
Nursing Process Application to ECG Monitoring
1. Assessment:
- Comprehensive cardiac assessment techniques
- Integration of ECG findings with patient history and presentation
- Using ECG as part of complete cardiovascular evaluation
- Decreased cardiac output related to dysrhythmias
- Activity intolerance related to cardiac disorders
- Acute pain related to myocardial ischemia
- Prioritizing care based on ECG findings and patient status
- Developing monitoring plans for different cardiac conditions
- Setting appropriate goals for cardiac rhythm management
- Evidence-based interventions for specific rhythm disturbances
- Delegation considerations for ECG monitoring
- Collaborative interventions with healthcare team
- Measuring effectiveness of interventions on cardiac rhythm
- Documenting patient response to treatment
- Modifying care plan based on changing ECG findings
Advanced Monitoring Considerations
1. 12-Lead ECG vs. Telemetry Monitoring:
- Indications for each monitoring method
- Nursing responsibilities specific to each approach
- Documentation differences between methods
- Temporary pacemaker monitoring
- Post-cardiac catheterization observation
- Post-cardioversion care
- Assessment parameters indicating readiness for discontinuation
- Documentation requirements for discontinuation
- Patient education upon monitoring completion
- Maintaining monitoring during patient transport
- Hand-off communication regarding rhythm status
- Equipment management during procedures
- Central monitoring station protocols
- Communication systems for urgent findings
- Documentation standards for remote monitoring
Patient and Family Teaching
1. Explanation of Cardiac Rhythm Abnormalities:
- Age-appropriate explanations of ECG findings
- Using visual aids for patient understanding
- Addressing common misconceptions
- Pulse check methods and documentation
- Recognition of symptoms requiring attention
- When to seek emergency care vs. routine follow-up
- Home monitoring equipment use
- Activity limitations with monitoring devices
- Troubleshooting common device issues
- Addressing anxiety related to cardiac rhythm disorders
- Family involvement in monitoring and care
- Coping strategies for living with cardiac conditions
- Support groups for cardiac patients
- Cardiac rehabilitation programs
- Home health services for continued monitoring
Special Population Considerations
1. Geriatric Patients:
- Normal age-related ECG changes
- Medication sensitivity and monitoring
- Skin integrity considerations with long-term monitoring
- Age-specific normal parameters
- Developmentally appropriate preparation
- Family-centered care approaches
- Normal physiologic changes affecting ECG
- Positioning considerations for monitoring
- Safe medication management
- Integration of ECG monitoring with other hemodynamic parameters
- Artifact reduction in complex care environments
- Prioritization of monitoring among multiple interventions
- Monitoring patients with agitation or confusion
- Managing anxiety related to cardiac monitoring
- Medication effects on cardiac conduction in psychiatric patients
Quality and Safety Considerations
1. Alarm Management:
- Preventing alarm fatigue
- Appropriate alarm parameter settings
- Institutional protocols for alarm response
- Routine checks and calibration
- Infection control practices
- Battery management for portable monitors
- Required elements of rhythm documentation
- Frequency of documentation based on patient condition
- Communication of significant findings
- Lead placement verification
- Patient identification protocols
- Artifact recognition and management
- Basic rhythm interpretation skills
- Emergency response protocols
- Ongoing education requirements
