NCLEX - Diabetes Mellitus Pathophysiology
Start your One-Week Free Trial
Already subscribed? Log in »
Here are key facts for NCLEX from the Diabetes Mellitus - Pathophysiology tutorial, as well as points of interest at the end of this document that are not directly addressed in this tutorial but should help you prepare for the boards. See the tutorial notes for further details and relevant links.
- --
VITAL FOR NCLEX
Diabetes Mellitus - Assessment & Recognition
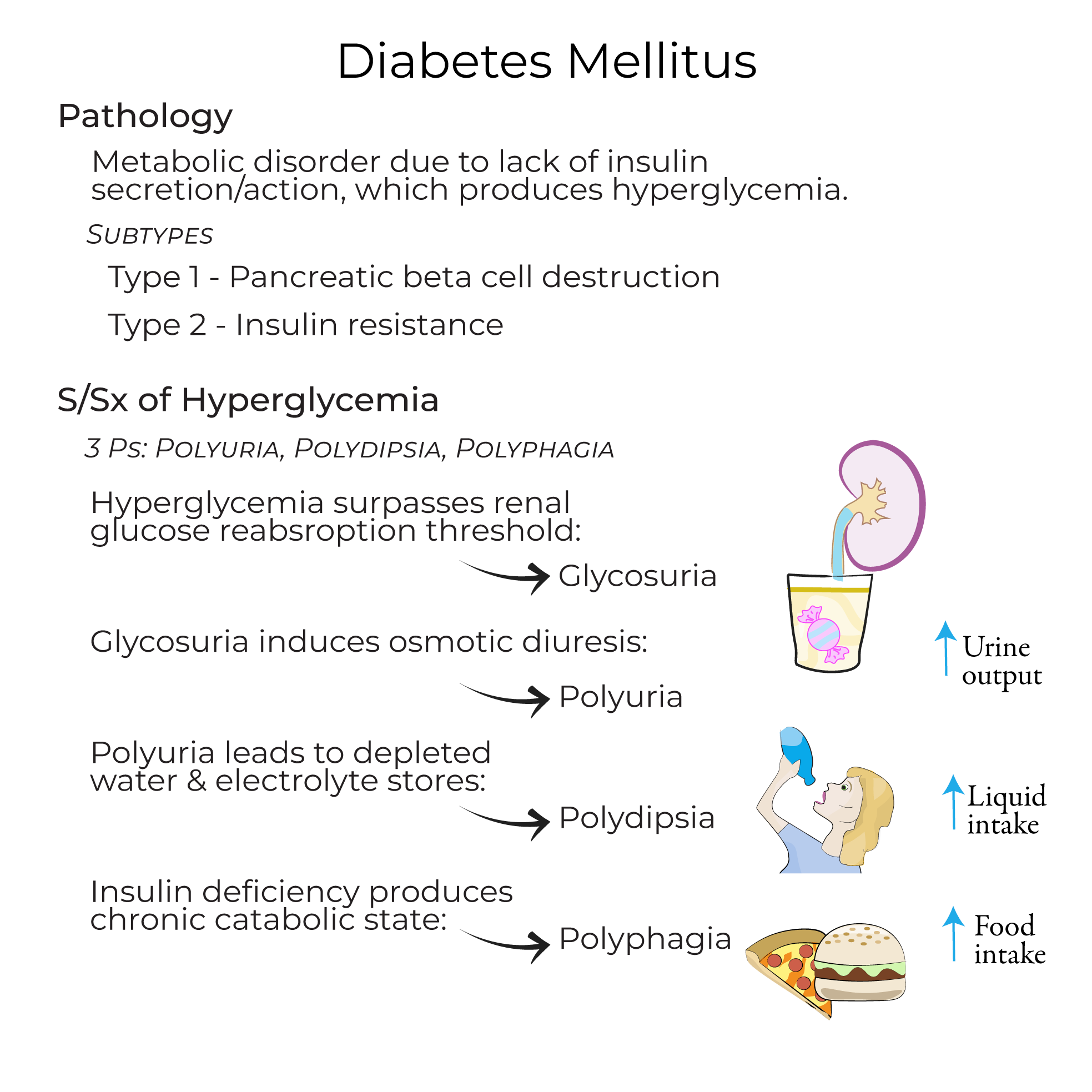
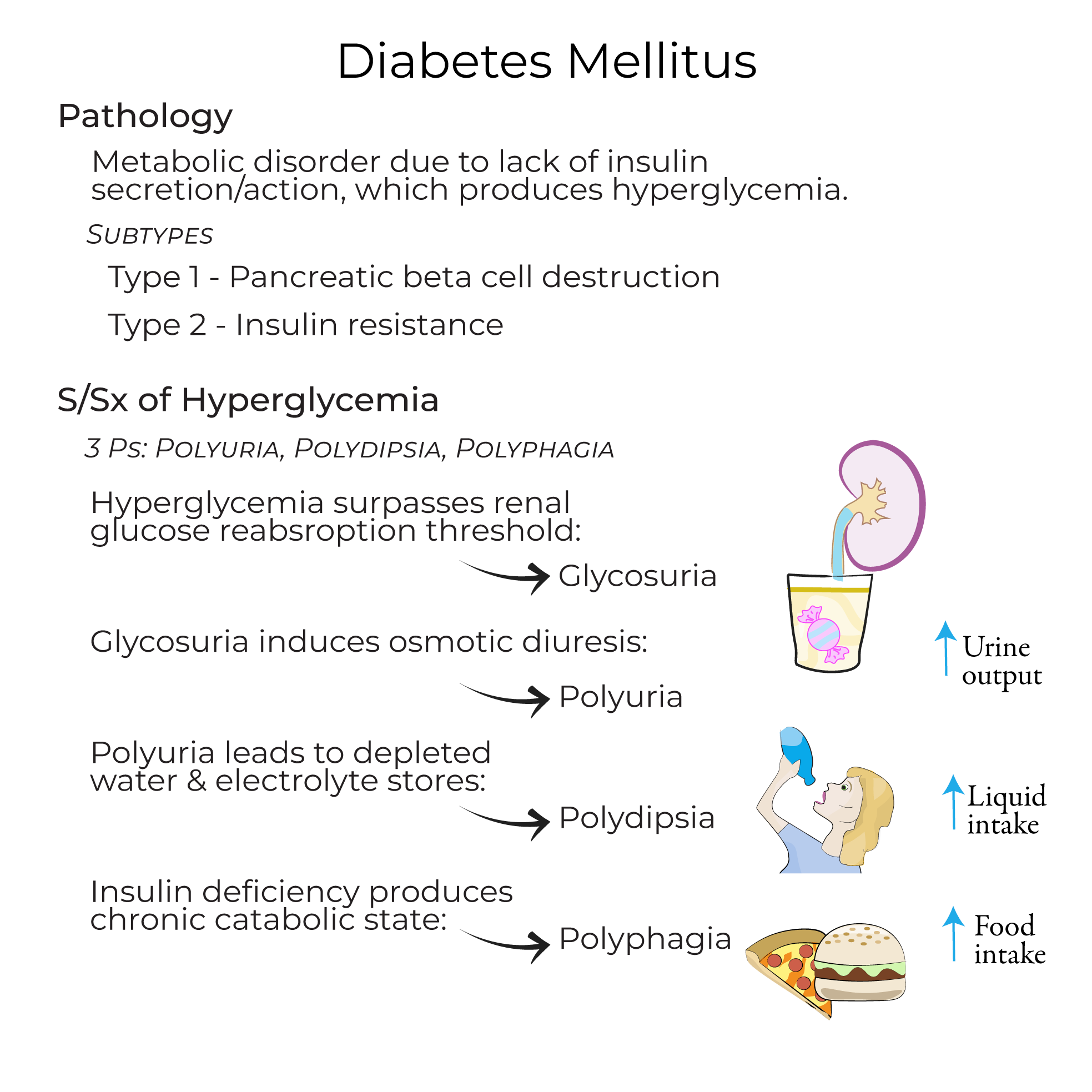
1. Definition & pathophysiology: A collection of metabolic disorders in which a lack of insulin secretion and/or insulin action leads to hyperglycemia.
2. Key diagnostic criteria: Assess for random plasma glucose level of 200+ mg/dL or a fasting plasma glucose level of 126+ mg/dL.
3. Classic signs & symptoms:
- Recognize the "3 P's": polyuria, polydipsia, and polyphagia
- Understand sequence: Glycosuria leads to osmotic diuresis (polyuria), causing depleted water and electrolyte stores (polydipsia), with increased hunger (polyphagia) from chronic catabolic state
Type 1 vs. Type 2 Diabetes - Nursing Considerations
1. Type 1 Diabetes:
- Population: Accounts for 5-10% of all diabetes mellitus cases
- Pathophysiology: Caused by autoimmune destruction of pancreatic beta cells
- Management: Requires exogenous insulin administration due to absolute insulin deficiency
- Complication risk: More prone to diabetic ketoacidosis
- Population: Represents 90-95% of all diabetes cases
- Pathophysiology: Characterized by peripheral tissue insulin resistance and relative insulin deficiency
- Risk factors: Associated with obesity, central fat distribution, sedentarism, stress, and inflammation
- Management approach: May include diet and exercise, Metformin, insulin, GLP-1 receptor agonists, or SGLT2-inhibitors
- Complication risk: More prone to Hyperosmolar Hyperglycemic Syndrome (HHS)
Acute Complications - Nursing Management
1. Diabetic Ketoacidosis (DKA):
- Assessment findings: Nausea and vomiting, fatigue, "fruity" odor, and Kussmal breathing
- Nursing interventions: Administer fluids, electrolytes, and insulin as prescribed
- High-risk patients: Those with polyuria and deficient water intake, particularly patients unable to drink on their own
- Critical awareness: Has a mortality rate of up to 20%
- Nursing interventions: Administer saline, insulin, and electrolytes as prescribed
- Assessment findings: Dizziness, sweating, palpitations, and tachycardia
- Causes: Missing a meal, excessive physical exertion, or excessive insulin administration
- Nursing intervention: Treat with glucose to correct the blood sugar levels
- --
HIGH YIELD
Patient Education & Health Promotion
1. Prediabetes education:
- Define condition: Glucose levels are elevated, but not high enough to be classified as diabetes
- Communicate risk: Pre-diabetic patients are at high risk for Type 2 diabetes and cardiovascular complications
- Emphasize prevention: Recommend increasing physical activity and losing weight
- Population context: The CDC reports that 1 in 3 Americans is pre-diabetic
- Exercise rationale: Exercise increases the number of Glut-4 receptors in skeletal muscle, improving insulin sensitivity
- Individualized approach: Treatment must be tailored to the individual and achievable glycemic targets
Medication Administration & Monitoring
1. Type 1 insulin management:
- Recognition of need: Required due to absolute insulin deficiency
- Variable requirements: Be aware that insulin needs may be variable, particularly in adults
- First-line therapy: Diet and exercise, and Metformin which decreases hepatic glucose production
- Additional agents: GLP-1 receptor agonists (increase rate of insulin secretion) or SGLT2-inhibitors (allow kidneys to eliminate excess glucose via urine)
- Patient factors: Consider that drugs can be costly and/or have contraindications
Complication Assessment & Monitoring
1. Vascular complications:
- Pathophysiology awareness: Results from chronic hyperglycemia
- Assessment focus:
- Macrovascular: Monitor for signs of heart failure and atherosclerosis
- Microvascular: Assess for kidney damage, visual impairment, and peripheral nerve dysfunction
- Pediatric patients: Monitor for impaired growth in children
- Infection risk: Assess for signs of infection due to immune suppression
- Type 1-specific: Be alert for signs of diabetic ketoacidosis
- Type 2-specific: Assess for HHS risk factors in patients unable to maintain adequate hydration
- --
Beyond the Tutorial
Nursing Process in Diabetes Care
1. Assessment: Comprehensive diabetes assessment including physical examination, nutrition evaluation, and psychosocial factors.
2. Nursing diagnosis: Common nursing diagnoses for patients with diabetes and their clinical applications.
3. Planning & implementation: Setting patient-centered goals and developing individualized care plans.
Skills & Procedures
1. Insulin administration: Techniques, sites, rotation, and prevention of lipohypertrophy.
2. Blood glucose monitoring: Correct technique, timing, and documentation.
3. Foot assessment: Comprehensive diabetic foot examination and patient teaching.
Patient Education & Self-Management
1. Sick day management: Guidelines for medication adjustment, fluid intake, and when to seek medical attention.
2. Hypoglycemia prevention & treatment: Signs, symptoms, and appropriate interventions including glucagon administration.
3. Nutritional guidance: Carbohydrate counting, meal planning, and dietary modifications.
Special Population Considerations
1. Pediatric diabetes care: Age-appropriate interventions and family education.
2. Geriatric considerations: Modified approaches to prevent hypoglycemia and falls.
3. Pregnancy: Monitoring and interventions for gestational and pre-existing diabetes.
