NCLEX - Cortisol Physiology & Pathology
Start your One-Week Free Trial
Already subscribed? Log in »
Here are key facts for NCLEX from the Cortisol Physiology & Pathology tutorial, as well as points of interest at the end of this document that are not directly addressed in this tutorial but should help you prepare for the boards. See the tutorial notes for further details and relevant links.
- --
VITAL FOR NCLEX
Pathophysiology and Assessment
1. Basic understanding: Cortisol is the primary glucocorticoid secreted by the zona fasciculata of the adrenal cortex and is triggered by ACTH from the anterior pituitary.
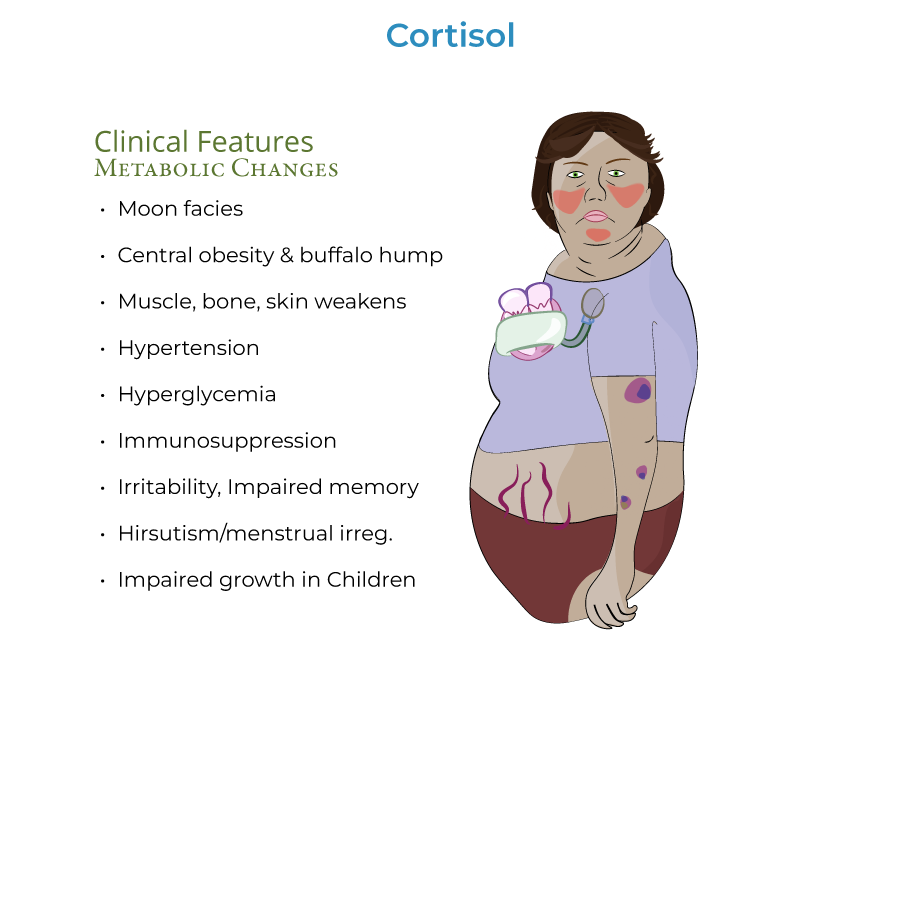
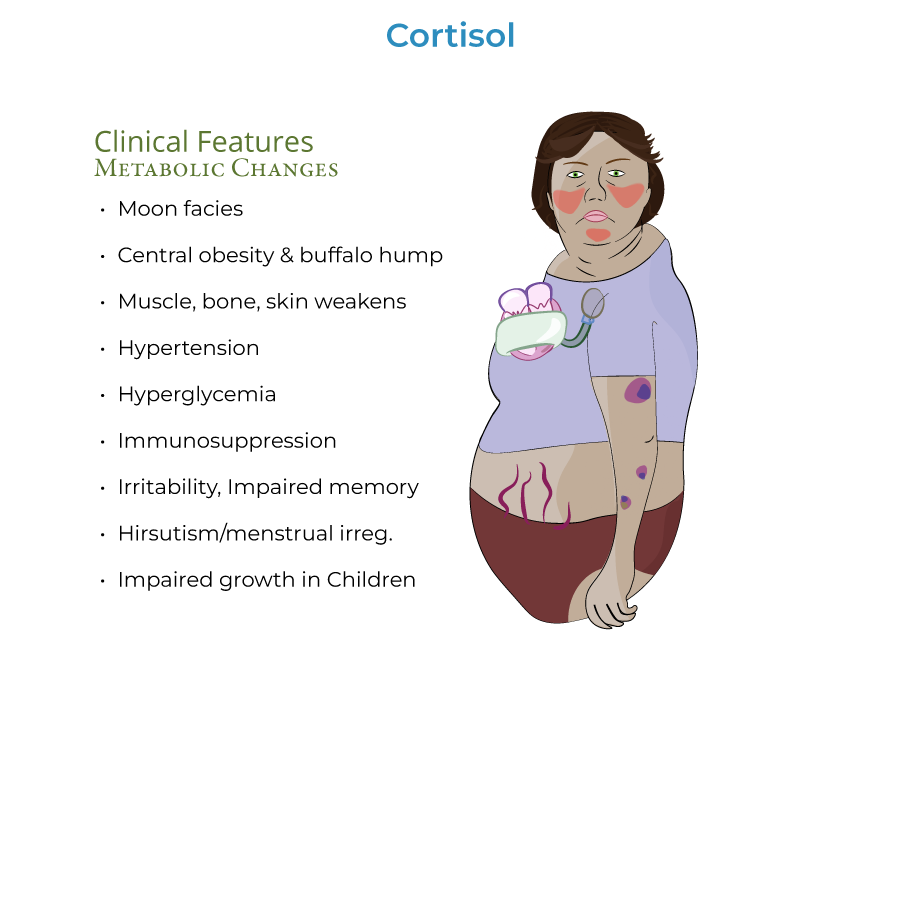
2. Definition: Cushing's Syndrome refers to elevated levels of cortisol, also known as hypercortisolism.
3. Classification: Hypercortisolism can be ACTH-dependent (caused by elevated ACTH) or ACTH-independent (not caused by elevated ACTH).
4. Common cause: Exogenous glucocorticoids are responsible for most cases of ACTH-independent hypercortisolism (iatrogenic Cushing's syndrome).
5. Key assessment findings: "Moon facies" (rounded face/neck from fat accumulation), central/truncal obesity with "buffalo hump," and red/purple striae on abdomen, breasts, thighs, and buttocks.
Clinical Manifestations
1. Body composition changes: Muscle atrophy particularly in extremities making limbs appear thin, while central obesity develops.
2. Skin manifestations: Red or purple striae, particularly on abdomen, breasts, thighs, and buttocks, and patients may bruise more easily.
3. Cardiovascular effects: Hypertension occurs via increased cardiac contractility and increased extracellular fluid volume.
4. Metabolic effects: Hyperglycemia that may progress to diabetes mellitus due to increased gluconeogenesis and insulin resistance.
5. Immune function: Immunosuppression increases vulnerability to infectious diseases that require robust B- and T-cell-mediated immune responses (tuberculosis, fungal infections).
Nursing Assessment Focus
1. History taking: Screen for causes of hypercortisolism, including exogenous glucocorticoid use, and rule out physiologic causes like pregnancy, alcoholism, anorexia, obesity, depression, and uncontrolled diabetes.
2. Physical examination: Assess for muscle atrophy, skin changes, fat distribution, and vital signs (especially blood pressure).
3. Diagnostic tests: Understand screening methods including 24-hour urine samples, midnight salivary samples, or dexamethasone suppression test.
4. Mental status: Monitor for emotional or psychiatric disturbances, such as irritability or impaired memory.
5. Complications: Watch for signs of fractures due to bone resorption and osteoporosis.
- --
HIGH YIELD
Nursing Care Priorities
1. Infection prevention: Due to immunosuppression, prioritize infection prevention measures for patients vulnerable to tuberculosis and fungal infections.
2. Blood glucose management: Monitor for hyperglycemia that may progress to diabetes mellitus.
3. Cardiovascular monitoring: Regularly assess blood pressure and other cardiovascular parameters due to hypertension risks.
4. Skin integrity: Assess and provide interventions for skin fragility, striae, and increased bruising.
5. Psychological support: Address potential emotional or psychiatric disturbances including irritability and impaired memory.
Medication-Related Nursing Considerations
1. Exogenous steroids: Most cases of Cushing's syndrome are due to exogenous glucocorticoid administration.
2. Cortisol regulation: Cortisol secretion is pulsatile and circadian with highest levels upon waking and lowest around bedtime.
3. Dexamethasone test: Dexamethasone is a synthetic glucocorticoid that mimics cortisol's negative feedback effects and is used diagnostically.
4. Plasma protein binding: Approximately 85% of cortisol in blood is bound to plasma proteins, giving it a long half-life.
5. Hormone interactions: Hypercortisolism affects other hormone systems, including suppression of thyrotropin, gonadotropin, and growth hormone.
Special Population Considerations
1. Pediatric patients: Hypercortisolism can impair linear growth in children via negative effects on bone growth and impaired hormone secretion.
2. Women's health: Monitor for hirsutism and menstrual irregularities due to excess androgen secretion in some forms of Cushing's syndrome.
3. Bone health: Assess for increased risk of fractures due to increased bone resorption and reduced formation of new bone tissue.
4. Stress response: Chronic physical and psychosocial stress can trigger cortisol secretion with widespread negative health effects.
5. Surgical patients: For patients with Cushing's Disease, treatment may involve removal of pituitary tumors or bilateral adrenalectomy.
- --
Beyond the Tutorial
Nursing Interventions
1. Fall prevention: Implement fall precautions due to muscle weakness, osteoporosis, and fracture risk.
2. Patient positioning: Use proper body mechanics and positioning to prevent skin breakdown in immobile patients.
3. Nutritional management: Collaborate with dietitians to manage weight changes, hyperglycemia, and increased metabolic demands.
4. Medication teaching: Educate patients about glucocorticoid medication regimens, tapering schedules, and avoiding abrupt discontinuation.
5. Post-surgical care: Monitor for complications following pituitary surgery or adrenalectomy, including adrenal insufficiency and electrolyte imbalances.
Patient Education
1. Self-monitoring: Teach patients to recognize and report signs of infection, changes in blood glucose, and bone pain.
2. Medication adherence: Stress importance of taking medications exactly as prescribed, especially for steroid replacement therapy.
3. Lifestyle modifications: Provide guidance on sodium restriction, regular exercise within limitations, and stress management techniques.
4. Medical alert identification: Encourage wearing medical alert identification for patients with adrenal insufficiency following treatment.
5. Long-term follow-up: Emphasize importance of regular medical follow-up and laboratory monitoring after treatment for Cushing's syndrome.
