NCLEX - Adrenal Insufficiency
Start your One-Week Free Trial
Already subscribed? Log in »
Here are key facts for the NCLEX from the Adrenal Insufficiency tutorial, as well as points of interest at the end of this document that are not directly addressed in this tutorial but should help you prepare for the boards. See the tutorial notes for further details and relevant links.
- --
VITAL FOR NCLEX
Adrenal Insufficiency (AI) Overview
1. High morbidity and mortality, especially when diagnosis is delayed.
2. Adrenal crisis is a medical emergency - suspect in patients with acute shock refractory to vasopressors and fluid replacement.
3. Primary AI (Addison's disease) affects all adrenal cortex hormones (cortisol, aldosterone, androgens).
4. Central AI primarily affects cortisol and androgen secretion, not aldosterone.
5. Treatment includes glucocorticoid replacement and mineralocorticoid replacement for primary AI.
Primary AI (Addison's Disease)
1. Hyperpigmentation of skin and mucosa is characteristic due to elevated ACTH.
2. Patients present with hypotension, hyponatremia, hyperkalemia, and metabolic acidosis.
3. Autoimmune diseases are the most common causes in the United States.
4. Acute adrenal crisis is life-threatening with shock, fever, dehydration, nausea, vomiting, hypoglycemia, apathy, and weakness.
5. Additional glucocorticoids are required during stressors like surgery to prevent crisis.
Central AI
1. More common than Primary AI.
2. No hyperpigmentation due to ACTH deficiency.
3. Less hypovolemia/hypotension because aldosterone secretion is normal.
4. Most commonly caused by long-term exogenous steroid use.
5. May be associated with deficiencies of other pituitary hormones.
- --
HIGH YIELD
Primary AI (Addison's Disease)
1. Autoimmune Polyendocrine Syndrome Type 1 (APS-1) presents in childhood with adrenal insufficiency, hypoparathyroidism, and mucocutaneous candidiasis.
2. Autoimmune Polyendocrine Syndrome Type 2 (APS-2) includes adrenal insufficiency, Hashimoto's thyroiditis, and Type I diabetes mellitus.
3. Infections like TB and HIV are important causes in endemic countries.
4. Symptoms include weakness, fatigue, weight loss, GI problems, and salt cravings.
5. Bilateral adrenal hemorrhage risk increases with anticoagulation therapy and conditions like antiphospholipid antibody syndrome.
Central AI
1. Symptoms are chronic and nonspecific due to glucocorticoid deficiencies.
2. May develop from sudden cessation of steroids or inability of HPA axis to respond to stressors.
3. Can be caused by pituitary or hypothalamic dysfunction including tumors, infections, and drugs.
4. Immune checkpoint inhibitors, high-dose progestins, and opioids can interrupt ACTH production.
5. Acute adrenal crisis can still occur despite normal aldosterone levels.
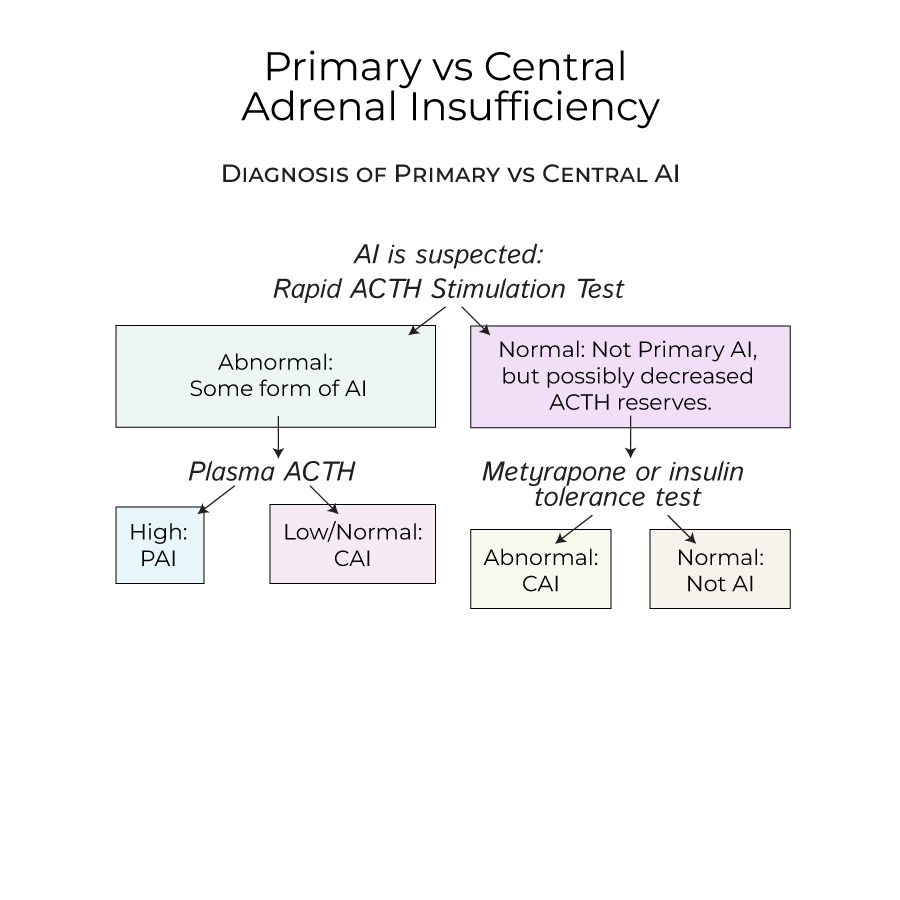
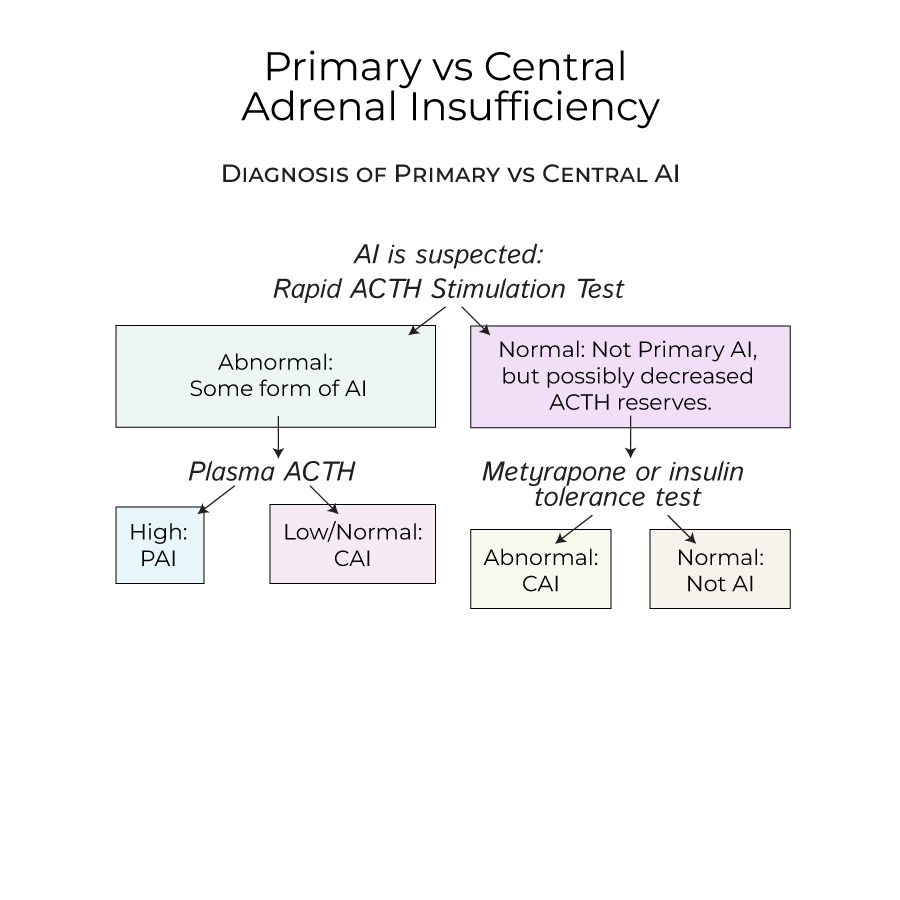
Diagnostic Testing
1. Rapid ACTH stimulation test is used when AI is suspected.
2. High plasma ACTH with abnormal cortisol response indicates Primary AI.
3. Low or normal plasma ACTH with abnormal cortisol response suggests Central AI.
4. Metyrapone or insulin tolerance tests can be used to test for Central AI.
5. Normal cortisol after testing excludes adrenal insufficiency.
- --
Beyond the Tutorial
Nursing Considerations
1. Monitor for signs of over-replacement of glucocorticoids (Cushing's syndrome).
2. Educate patients on carrying medical alert cards/jewelry to indicate adrenal insufficiency.
3. Be vigilant for Waterhouse-Friderichsen Syndrome in children with meningococcal or pseudomonas infections.
4. Recognize that John F Kennedy Jr. had the characteristic "bronzed" appearance of Addison's Disease.
5. Understand the multidisciplinary approach needed for patients with polyendocrine syndromes.
Critical Nursing Interventions
1. Prioritize recognition of adrenal crisis as a medical emergency requiring immediate intervention.
2. Assess fluid status carefully in AI patients who may be severely dehydrated.
3. Monitor electrolytes closely, especially sodium and potassium levels.
4. Administer stress-dose steroids before procedures or during illness.
5. Provide patient education about lifelong hormone replacement therapy.
