Asthma for ABIM
Start your One-Week Free Trial
Already subscribed? Log in »
Asthma for the American Board of Internal Medicine Exam
Pathophysiology
- Chronic Inflammation:
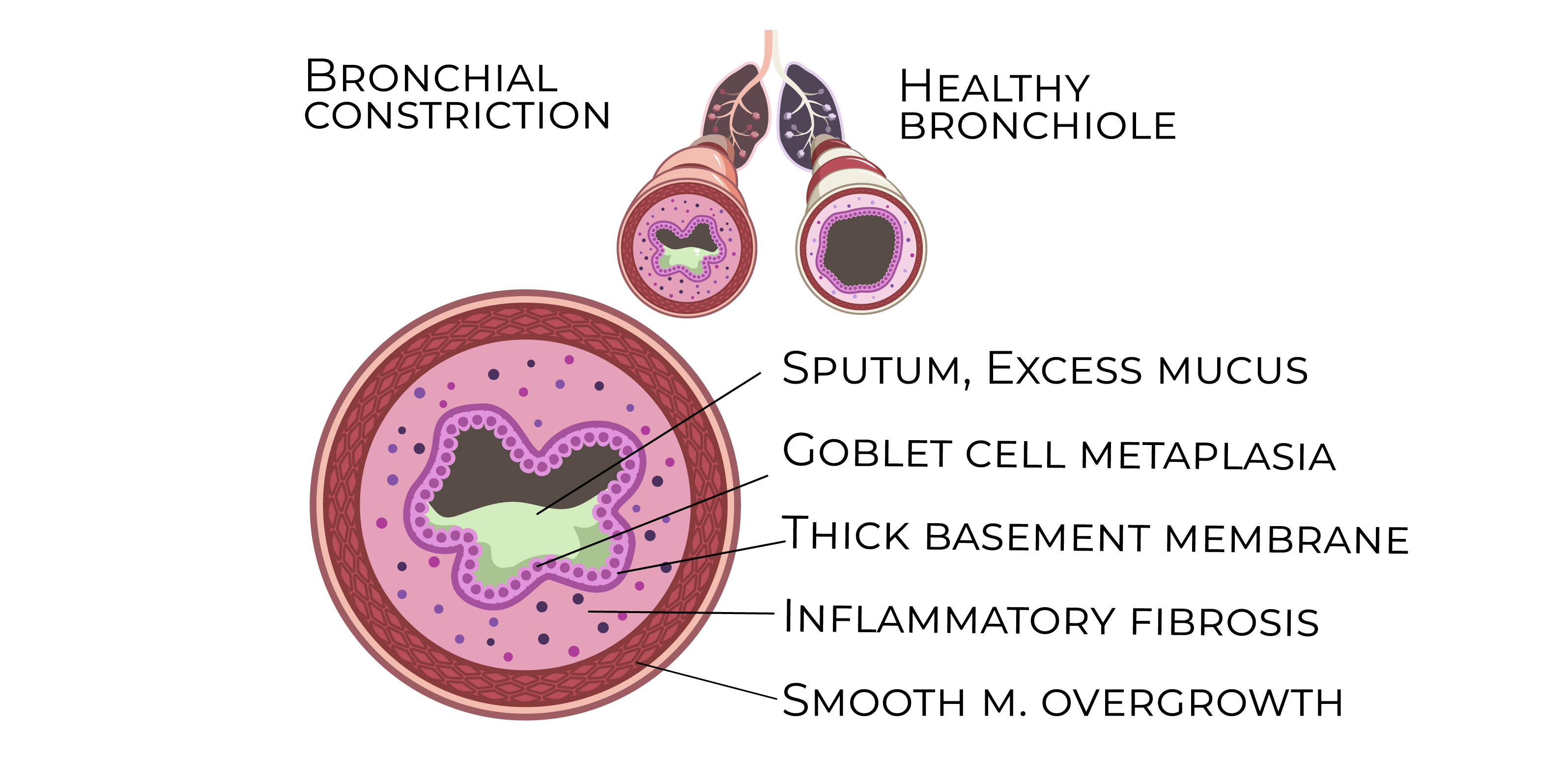
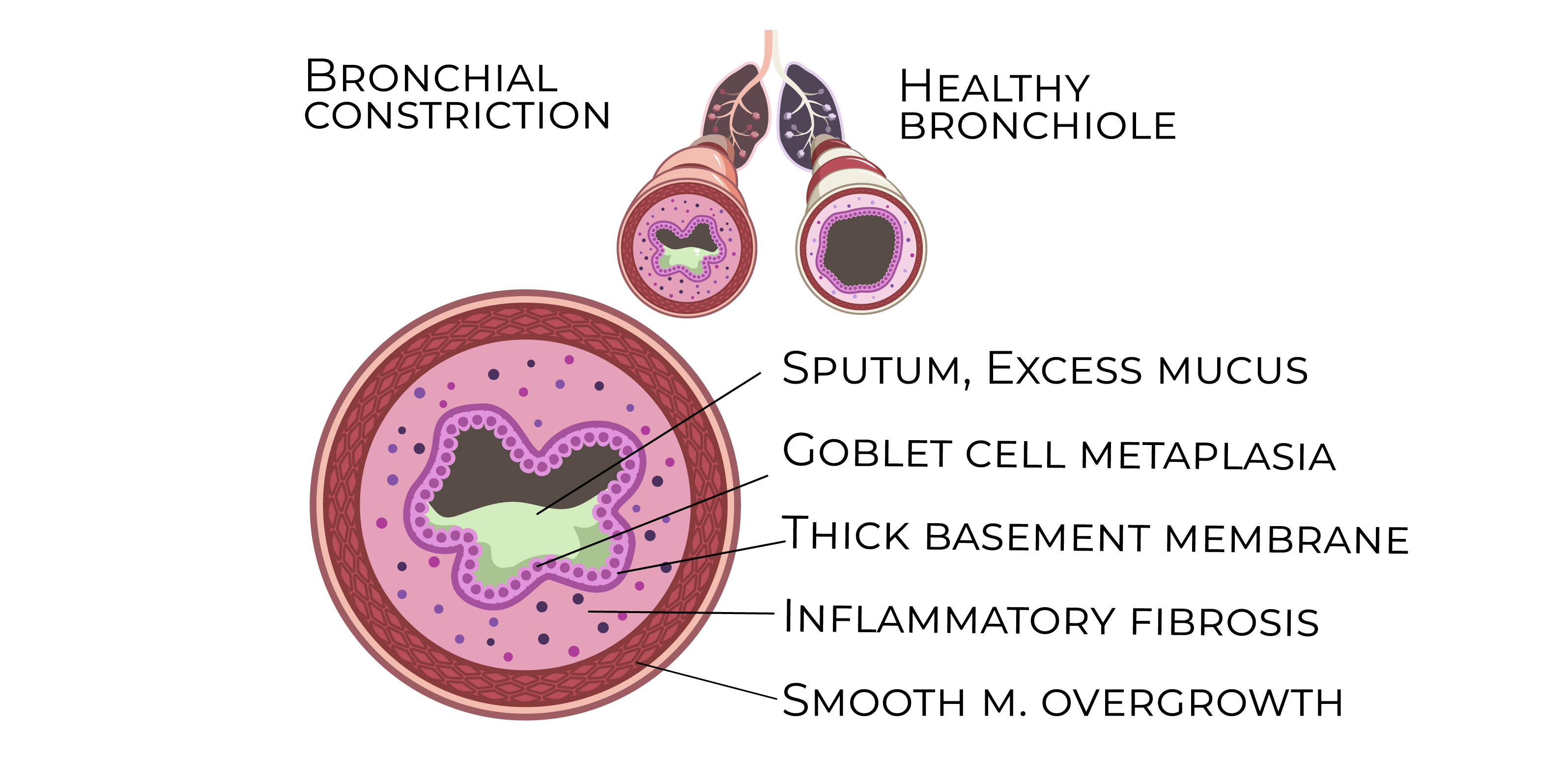
- Asthma is a chronic inflammatory disease of the airways characterized by the activation of mast cells, eosinophils, T-helper 2 (Th2) cells, and cytokines (IL-4, IL-5, IL-13). This inflammatory response leads to airway hyperreactivity, bronchoconstriction, and remodeling.
- The inflammation causes recurrent episodes of wheezing, breathlessness, chest tightness, and coughing, especially at night or early morning.
- Airway Hyperresponsiveness:
- In asthmatic patients, the airways overreact to various stimuli such as allergens, cold air, or exercise. This hyperresponsiveness results in bronchospasm and airflow limitation.
- Airway Remodeling:
- Over time, repeated inflammation leads to structural changes in the airway, including smooth muscle hypertrophy, goblet cell hyperplasia, and subepithelial fibrosis. These changes can cause irreversible airflow limitation if not managed effectively.
- Immunologic Mechanisms:
- Asthma involves both innate and adaptive immune responses. IgE-mediated allergic reactions are central to many cases, with allergens binding to IgE on mast cells, releasing histamines, leukotrienes, and other inflammatory mediators that cause bronchoconstriction.
Risk Factors
- Genetics:
- A family history of asthma or atopic diseases (e.g., allergic rhinitis, eczema) increases the risk of developing asthma.
- Environmental Exposures:
- Common asthma triggers include:
- Allergens: Pollen, dust mites, pet dander, and molds.
- Occupational Exposures: Chemical fumes, dust, or occupational allergens.
- Smoking: Both active and passive smoking increase asthma risk.
- Viral Infections:
- Respiratory infections, particularly in early childhood (e.g., respiratory syncytial virus [RSV]), are linked to the development of asthma.
Clinical Features
- Intermittent Wheezing:
- Expiratory wheezing is the hallmark symptom of asthma. It may occur during exacerbations or in response to triggers.
- Shortness of Breath:
- Patients experience dyspnea that is usually episodic, often worse at night or early morning.
- Chest Tightness:
- Patients may describe a sensation of chest tightness or discomfort, especially during exacerbations.
- Cough:
- A nonproductive cough, often worse at night, is a common feature of asthma.
- Exacerbations:
- Acute worsening of symptoms can be triggered by infections, allergens, or exercise, leading to increased use of rescue medications.
Diagnosis
- Spirometry:
- Spirometry is the main diagnostic tool for asthma and is used to assess the degree of airflow limitation and response to bronchodilators:
- Reduced FEV1: Indicates airflow obstruction.
- FEV1/FVC ratio: Decreased, but improves after bronchodilator administration.
- Bronchodilator Response: An increase in FEV1 by at least 12% and 200 mL after using a short-acting beta-agonist confirms the diagnosis.
- Peak Expiratory Flow (PEF):
- PEF measurements can be used to monitor asthma control. A reduction in PEF indicates worsening asthma or impending exacerbation.
- Methacholine Challenge Test:
- In patients with normal spirometry but suspected asthma, a methacholine challenge can provoke bronchoconstriction, with a positive test indicating increased airway reactivity.
- Allergy Testing:
- Skin or serum-specific IgE tests may identify allergens that trigger asthma in allergic patients.
Management
Stepwise Treatment Approach:
- Intermittent Asthma (Step 1):
- Short-acting beta-agonists (SABAs): Albuterol as needed for symptom relief.
- Mild Persistent Asthma (Step 2):
- Low-dose inhaled corticosteroids (ICS): First-line maintenance therapy.
- Leukotriene receptor antagonists (LTRAs): Alternatives for patients who cannot tolerate ICS or prefer oral therapy.
- Moderate Persistent Asthma (Step 3):
- Low-dose ICS + Long-acting beta-agonists (LABAs): Combination therapy for patients who require more control.
- Medium-dose ICS: An alternative for patients who cannot tolerate LABAs.
- Severe Persistent Asthma (Step 4 and above):
- Medium-dose ICS + LABA or High-dose ICS + LABA: For patients with severe symptoms.
- Add-on Therapies: Consider tiotropium (a long-acting muscarinic antagonist), omalizumab (for allergic asthma), or biologics (anti-IL-5, anti-IL-4).
Acute Exacerbation Management:
- SABAs:
- Albuterol or levalbuterol via metered-dose inhaler or nebulizer is the first-line treatment for exacerbations.
- Systemic Corticosteroids:
- Oral prednisone or intravenous methylprednisolone is used to reduce inflammation during moderate-to-severe exacerbations.
- Oxygen Therapy:
- Administered in severe exacerbations to maintain oxygen saturation above 90%.
- Magnesium Sulfate:
- Intravenous magnesium sulfate is used as an adjunct in life-threatening exacerbations unresponsive to conventional therapy.
Asthma Control and Monitoring
- Asthma Control Test (ACT):
- A validated questionnaire used to assess asthma control in patients. A score ≥20 indicates well-controlled asthma.
- Peak Flow Monitoring:
- Patients can monitor their PEF daily to detect early signs of worsening asthma or exacerbations.
- Inhaler Technique and Adherence:
- Correct inhaler technique and adherence to prescribed medications are essential for effective asthma management.
- Environmental Control:
- Reducing exposure to known allergens (e.g., dust mites, pet dander) and irritants (e.g., tobacco smoke) is critical for asthma control.
Complications
- Status Asthmaticus:
- A severe, life-threatening asthma exacerbation unresponsive to standard treatments, requiring intensive care and possible mechanical ventilation.
- Airway Remodeling:
- Repeated episodes of inflammation and poor asthma control can lead to permanent airway changes and fixed airflow limitation.
- Pneumothorax:
- Rare but serious complication during severe exacerbations, especially with overuse of bronchodilators.
Key Points
- Asthma is a chronic inflammatory disease with airway hyperresponsiveness and episodic symptoms like wheezing, dyspnea, cough, and chest tightness.
- Risk factors include family history, environmental exposures, and viral infections in childhood.
- Diagnosis is confirmed through spirometry, showing reversible airway obstruction (FEV1/FVC ratio improvement with bronchodilator use).
- Asthma management follows a stepwise approach, starting with SABAs for intermittent asthma and escalating to ICS, LABAs, and biologics for persistent disease.
- Acute exacerbations are managed with SABAs, systemic corticosteroids, and, in severe cases, oxygen therapy or magnesium sulfate.
- Monitoring of asthma control using tools like the Asthma Control Test (ACT) and peak flow monitoring is essential for adjusting treatment and preventing exacerbations.
- Complications include status asthmaticus, airway remodeling, and, in rare cases, pneumothorax.
