Allergy & Hypersensitivity for ABIM
Start your One-Week Free Trial
Already subscribed? Log in »
Allergy for the American Board of Internal Medicine Exam
Allergy Overview
- Definition:
- Allergies are hypersensitivity reactions involving the immune system, characterized by excessive immune responses to non-harmful antigens (allergens).
- Mediated by IgE antibodies that trigger mast cell and basophil degranulation, leading to the release of histamine and other inflammatory mediators.
- Common Allergens:
- Environmental: Pollens, dust mites, animal dander, molds.
- Food: Common allergens include peanuts, tree nuts, shellfish, milk, eggs, and wheat.
- Insect Stings: Hymenoptera (e.g., bees, wasps).
- Medications: Antibiotics (penicillin), NSAIDs, and vaccines in some cases.
- Occupational: Latex, chemicals, and workplace allergens.
Mechanisms of Hypersensitivity
- Type I (IgE-Mediated) Hypersensitivity:
- Pathophysiology: Initial exposure sensitizes the immune system, leading to IgE antibody production. Upon re-exposure, IgE cross-links on mast cells and basophils, causing degranulation and release of histamine, prostaglandins, and leukotrienes.
- Examples: Allergic rhinitis, asthma, food allergies, anaphylaxis.
- Type II (Cytotoxic) Hypersensitivity:
- Pathophysiology: IgG or IgM antibodies target antigens on cell surfaces, activating the complement system and resulting in cell lysis.
- Examples: Hemolytic reactions, Goodpasture syndrome, autoimmune hemolytic anemia.
- Type III (Immune Complex-Mediated) Hypersensitivity:
- Pathophysiology: Formation of antigen-antibody complexes that deposit in tissues, leading to inflammation and tissue damage through complement activation.
- Examples: Serum sickness, systemic lupus erythematosus (SLE), and some forms of vasculitis.
- Type IV (Delayed-Type) Hypersensitivity:
- Pathophysiology: T-cell mediated response that occurs 24-72 hours after exposure, with cytokine release and macrophage activation.
- Examples: Contact dermatitis, tuberculosis skin test reaction, and some drug hypersensitivity reactions.
Clinical Presentation of Allergic Reactions
- Allergic Rhinitis:
- Symptoms: Sneezing, nasal congestion, rhinorrhea, itchy eyes, and throat. Often seasonal with pollen allergies or perennial with dust mites or mold.
- Diagnosis: Based on history, physical examination, and skin or serum IgE testing for specific allergens.
- Treatment: Intranasal corticosteroids, antihistamines, decongestants, and allergen avoidance.
- Asthma:
- Symptoms: Cough, wheezing, shortness of breath, and chest tightness, often triggered by allergens.
- Diagnosis: Pulmonary function tests (PFTs) showing reversible airflow obstruction; IgE testing may identify triggers.
- Treatment: Inhaled corticosteroids, bronchodilators, leukotriene receptor antagonists, and allergen avoidance.
- Atopic Dermatitis:
- Symptoms: Pruritic, erythematous, scaly rash often on flexural surfaces in children and adults.
- Diagnosis: Based on clinical features, family history, and allergy testing for environmental and food triggers if suspected.
- Treatment: Emollients, topical corticosteroids, and in severe cases, immunomodulators (e.g., tacrolimus, dupilumab).
- Food Allergy:
- Symptoms: Urticaria, angioedema, gastrointestinal symptoms (nausea, vomiting, diarrhea), respiratory symptoms, and anaphylaxis in severe cases.
- Diagnosis: Skin prick testing, serum IgE testing, and oral food challenges.
- Treatment: Strict avoidance of allergens and use of epinephrine autoinjectors for anaphylactic reactions.
- Drug Allergy:
- Symptoms: Ranges from mild (rash, urticaria) to severe (anaphylaxis, Stevens-Johnson syndrome).
- Diagnosis: Based on history, skin testing (e.g., penicillin), and drug challenge.
- Treatment: Avoidance, substitution with non-cross-reactive drugs, and desensitization when alternatives are unavailable.
- Anaphylaxis:
- Symptoms: Sudden, severe, multisystem reaction characterized by urticaria, angioedema, bronchospasm, hypotension, and shock.
- Common Triggers: Foods, insect stings, medications.
- Diagnosis: Clinical diagnosis based on acute presentation with exposure to a known allergen.
- Treatment: Immediate intramuscular epinephrine, followed by antihistamines, corticosteroids, and supportive care. Patients should carry an epinephrine autoinjector.
Diagnostic Approaches
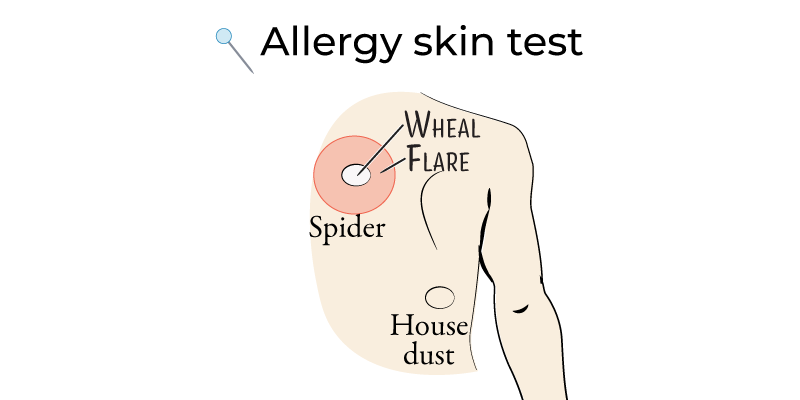
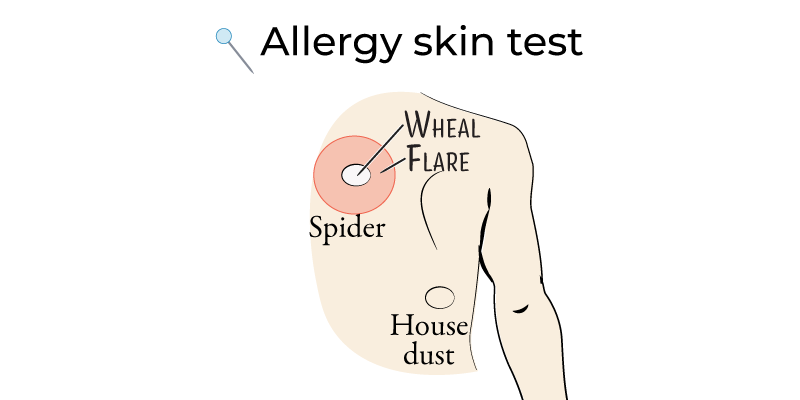
- Skin Prick Testing:
- Procedure: Small amounts of allergens are introduced into the skin; a wheal and flare response indicates sensitization.
- Indications: Allergic rhinitis, asthma, atopic dermatitis, and food allergies.
- Limitations: Contraindicated in patients with severe anaphylactic reactions to specific allergens.
- Serum IgE Testing:
- Procedure: Measures specific IgE antibodies against allergens in the blood.
- Indications: Useful in patients unable to undergo skin testing (e.g., severe skin conditions, those on antihistamines).
- Limitations: Lower sensitivity than skin testing and may not correlate directly with symptom severity.
- Oral Food Challenge:
- Procedure: Controlled exposure to suspect food allergen under medical supervision.
- Indications: Gold standard for diagnosing food allergy; used when skin or IgE testing is inconclusive.
- Limitations: Risk of triggering severe allergic reactions; should be performed in a controlled setting.
- Challenge Testing for Drug Allergy:
- Procedure: Incremental dosing of the suspected drug under close monitoring.
- Indications: Used for drugs with a high likelihood of cross-reactivity when alternatives are not available.
- Limitations: Risk of anaphylaxis; requires expertise and emergency preparedness.
Management Strategies
- Avoidance and Allergen Control:
- Environmental Allergens: Use of air purifiers, removing carpeting, and regular cleaning to reduce dust mites, pet dander, and mold.
- Food Allergies: Label reading and avoidance strategies; education on cross-contamination prevention.
- Drug Allergies: Avoidance of specific drugs and using alternatives when available.
- Pharmacologic Management:
- Antihistamines: First-line for allergic rhinitis, urticaria, and mild allergic reactions.
- Corticosteroids: Intranasal for rhinitis, inhaled for asthma, topical for atopic dermatitis, and systemic for severe reactions.
- Bronchodilators: Short-acting beta agonists for asthma symptoms.
- Leukotriene Receptor Antagonists: Adjunctive therapy for allergic rhinitis and asthma.
- Immunotherapy:
- Subcutaneous Immunotherapy (SCIT): Regular allergen injections to induce tolerance over time.
- Sublingual Immunotherapy (SLIT): Oral administration of allergens, especially for pollen and dust mite allergies.
- Indications: Allergic rhinitis, asthma, insect sting allergy.
- Limitations: Requires several years of treatment; risk of systemic reactions.
- Emergency Preparedness for Anaphylaxis:
- Patients with a history of anaphylaxis should carry an epinephrine autoinjector and receive education on recognizing symptoms and using the device.
- Family members and caregivers should also be educated on anaphylaxis management and emergency response.
Key Points
- Allergies are immune-mediated hypersensitivity reactions, primarily IgE-driven (Type I) but can include other types, each with distinct pathophysiology and examples.
- Clinical presentation varies by allergen and route of exposure; common presentations include allergic rhinitis, asthma, atopic dermatitis, food and drug allergies, and anaphylaxis.
- Diagnosis involves history, physical exam, and allergen-specific testing (skin prick, serum IgE, and challenge testing).
- Management focuses on allergen avoidance, pharmacologic treatment (e.g., antihistamines, corticosteroids), and immunotherapy.
- Anaphylaxis requires immediate treatment with epinephrine, and at-risk patients should be equipped with an epinephrine autoinjector and education on its use.
- Immunotherapy is effective for some allergens and requires long-term commitment; it is not without risk and should be monitored closely.
