ABIM - Valvular Disease
Start your One-Week Free Trial
Already subscribed? Log in »
Here are key facts for ABIM from the Valvular Disease tutorial, as well as points of interest at the end of this document that are not directly addressed in this tutorial but should help you prepare for the boards. See the tutorial notes for further details and relevant links.
1. Stenosis vs. Regurgitation:
Stenosis*: Obstruction of forward blood flow due to narrowed valve orifice.
Regurgitation/Insufficiency*: Incomplete valve closure allows reverse flow.
2. Aortic Stenosis – Most Common Degenerative Valve Disease:
 11. AV Valve Support:
15. Hydroxyapatite Role in Valve Calcification:
11. AV Valve Support:
15. Hydroxyapatite Role in Valve Calcification:
 17. Mitral Valve Morphology:
21. Murmur Identification & Clinical Clues:
Aortic stenosis*: systolic crescendo–decrescendo murmur; radiates to carotids.
Mitral regurgitation*: holosystolic murmur at apex; radiates to axilla.
Aortic regurgitation*: high-pitched, early diastolic murmur at LSB.
Mitral stenosis*: opening snap + low-pitched diastolic rumble at apex.
22. Workup of Suspected Valve Disease:
17. Mitral Valve Morphology:
21. Murmur Identification & Clinical Clues:
Aortic stenosis*: systolic crescendo–decrescendo murmur; radiates to carotids.
Mitral regurgitation*: holosystolic murmur at apex; radiates to axilla.
Aortic regurgitation*: high-pitched, early diastolic murmur at LSB.
Mitral stenosis*: opening snap + low-pitched diastolic rumble at apex.
22. Workup of Suspected Valve Disease:
- --
VITAL FOR ABIM
- Caused by calcific degeneration and hydroxyapatite deposition on cusps.
- Mimics bone formation due to osteoblast-like cell activity.
- Congenital in \~1% of population.
- Accelerates valve degeneration due to increased mechanical stress.
- Characteristic “buttonhole” or “fish mouth” deformity.
- Leads to fusion of leaflets and chordae tendineae.
- Prolapse into LA during systole due to weakened support structures.
- Leads to regurgitation, stroke risk, and progressive calcification.
- Causes include Marfan syndrome, hypertension, and aneurysm.
- Alters wall stress and may remain asymptomatic until advanced.
- Occurs at the annular ring, not the leaflets.
- Associated with stroke, arrhythmias, and infective endocarditis.
- Mechanical valves: high thromboembolism risk → lifelong anticoagulation (e.g., warfarin).
- Bioprosthetic valves: less thrombogenic, but degenerate sooner.
- Valve disease and prosthetics increase risk.
- Prophylaxis recommended before gingival-damaging procedures.
- Aortic valve: right coronary, left coronary, and posterior non-coronary cusps.
- Mitral valve: anterior and posterior cusps, subdivided A1–A3, P1–P3.
- Tricuspid valve: anterior, posterior, and septal leaflets.
 11. AV Valve Support:
11. AV Valve Support:
- Leaflets anchored by chordae tendineae and papillary muscles.
- Disruption leads to functional mitral regurgitation, particularly post-MI.
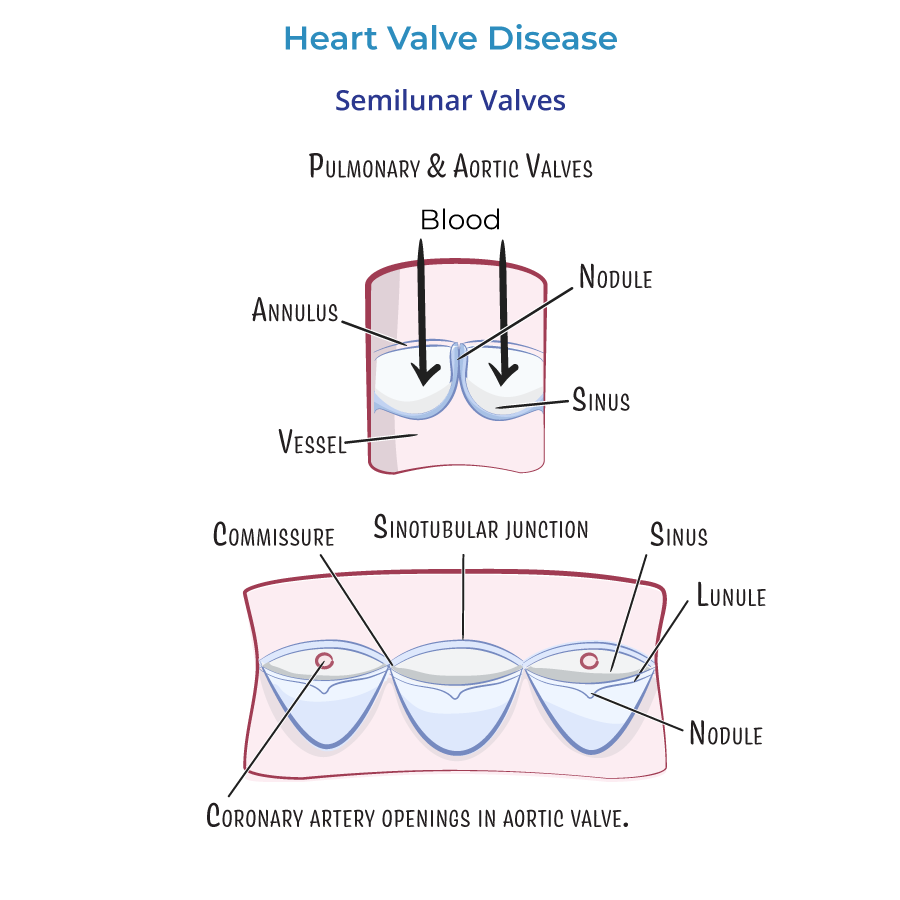
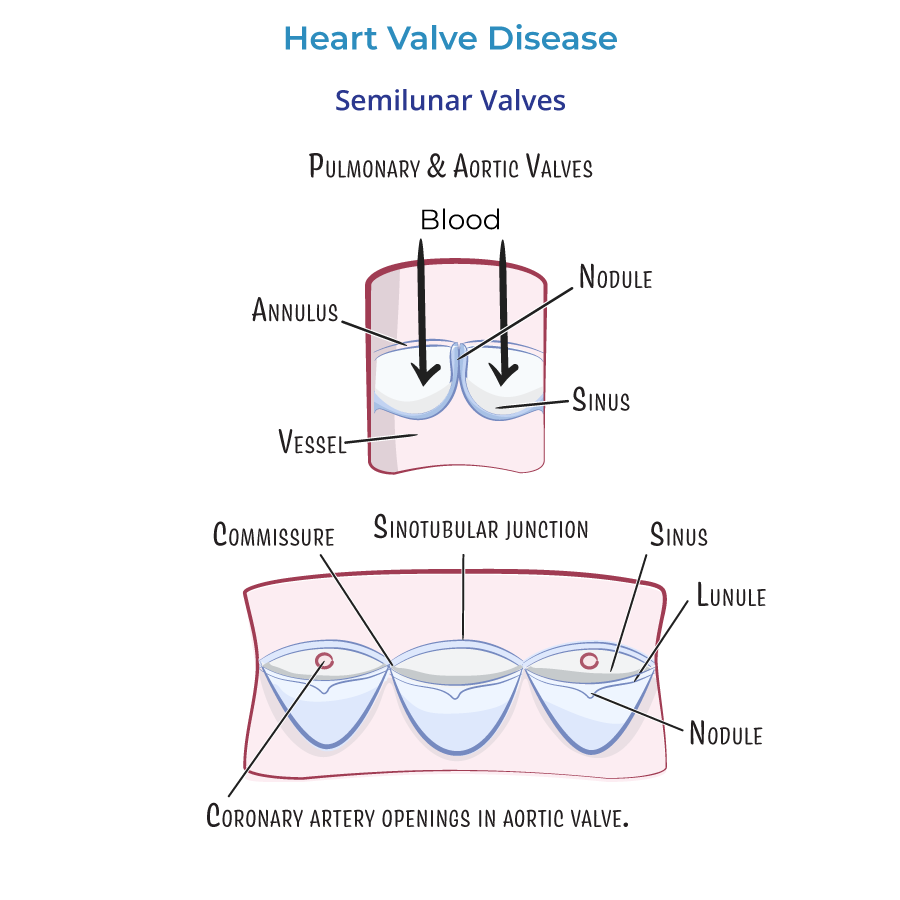
- Prevent backflow during diastole by trapping blood in sinuses.
- Includes nodule of Arantius, lunule, commissures, and sinotubular junction.
- Calcification and irregular flow patterns increase embolic stroke risk.
- Coronary arteries arise from the right and left aortic sinuses.
- --
HIGH YIELD
- Same calcium salt as found in bone; indicates osteogenic activity in valve degeneration.
 17. Mitral Valve Morphology:
17. Mitral Valve Morphology:
- Comprises anterior and posterior leaflets, each with three named segments.
- Important for surgical repair planning and TTE/TEE localization.
- Caused by disruption of valve support, not valve structure itself (e.g., post-MI papillary muscle rupture).
- Leaflets become rubbery and thick due to spongiosa expansion.
- Often found in chronic mitral prolapse or with connective tissue disorders.
- The heart contracts over 30 million times per year, progressively deforming and injuring valve tissue.
- --
Beyond the Tutorial
- TTE is initial test.
- Use TEE for prosthetic valve evaluation or to exclude endocarditis.
- Order BNP, ECG, and chest X-ray if HF is suspected.
- Prefer bioprosthetic valves in women of childbearing age to avoid warfarin.
- Mitral stenosis may worsen with volume expansion during pregnancy.
- Target INR:
- Mechanical AVR: 2.0–3.0.
- Mechanical MVR or dual valves: 2.5–3.5.
- Regular echo follow-up to assess structural deterioration or complications.
- May appear less severe on echo due to low cardiac output.
- Use dobutamine stress echo to assess true severity.
- Primarily for mitral stenosis with favorable valve morphology and no LA thrombus.
- Indicated for high-risk patients:
- Prosthetic heart valves
- History of infective endocarditis
- Certain congenital heart diseases
- Cardiac transplant recipients with valve disease
- Papillary muscle rupture → acute severe mitral regurgitation → surgical emergency.
