ABIM - Pulmonary Embolism and Deep Vein Thrombosis
Start your One-Week Free Trial
Already subscribed? Log in »
Here are key facts for American Board of Internal Medicine (ABIM) Examination from the Pulmonary Embolism & Deep Vein Thrombosis tutorial, focusing on clinical management and treatment decision-making that are essential for board certification. See the tutorial notes for further details and relevant links.
 4. Nonthrombotic Emboli: Air, fat, amniotic fluid, bacterial (septic), foreign bodies, and tumors can also cause PE.
5. Key Complications: Pulmonary hypertension, right heart failure, and pulmonary infarction.
4. Nonthrombotic Emboli: Air, fat, amniotic fluid, bacterial (septic), foreign bodies, and tumors can also cause PE.
5. Key Complications: Pulmonary hypertension, right heart failure, and pulmonary infarction.
 2. Combined Risk Assessment: Patients with multiple predisposing factors have significantly higher risk (e.g., pregnant women on bed rest).
3. Risk Stratification for PE:
Below is information not explicitly contained within the tutorial but important for the American Board of Internal Medicine Examination.
2. Combined Risk Assessment: Patients with multiple predisposing factors have significantly higher risk (e.g., pregnant women on bed rest).
3. Risk Stratification for PE:
Below is information not explicitly contained within the tutorial but important for the American Board of Internal Medicine Examination.
- --
VITAL FOR ABIM
Pathophysiology & Clinical Significance
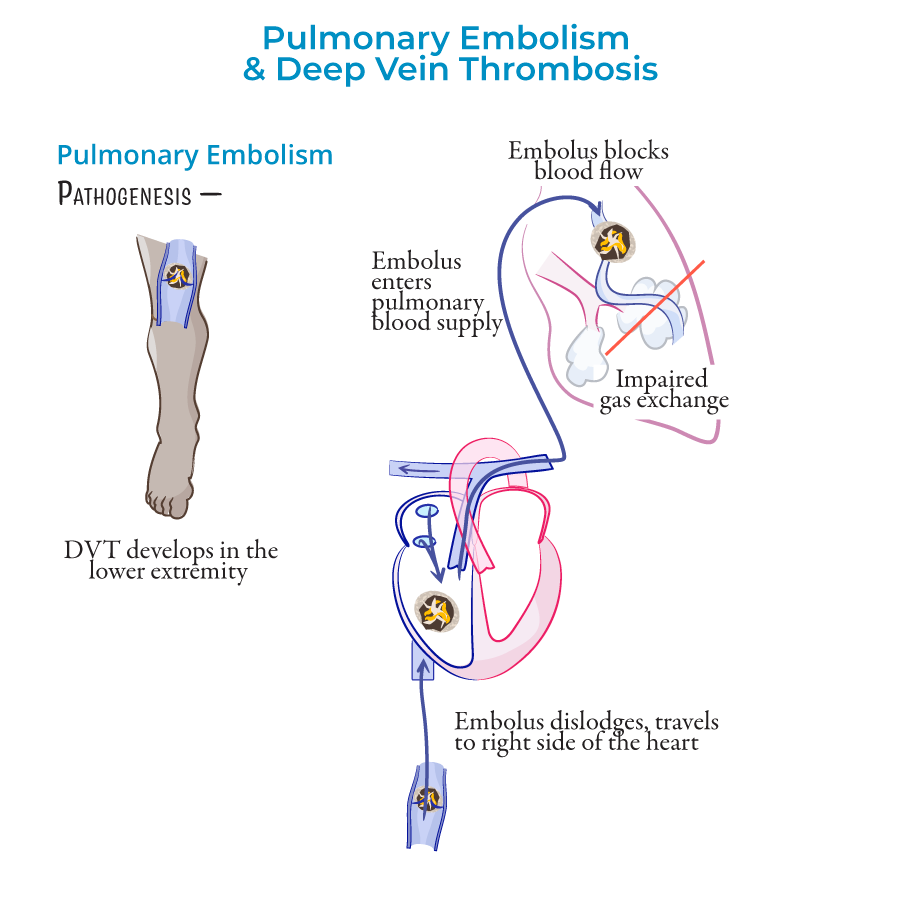
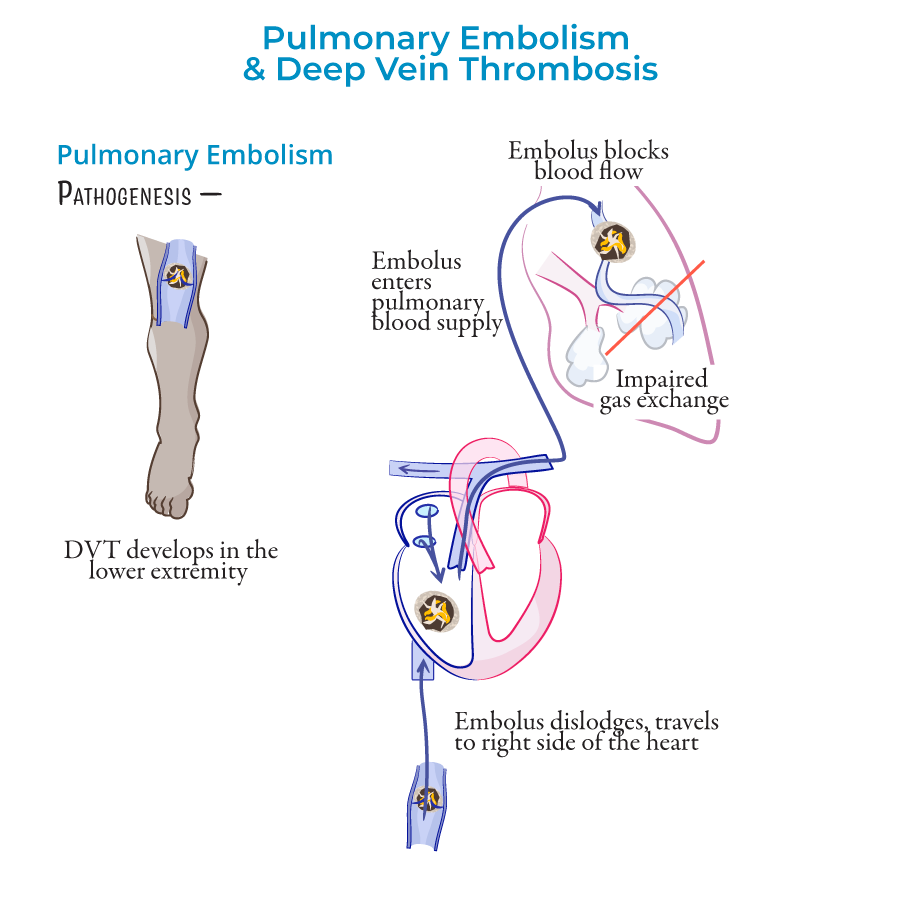
1. Definition & Relationship: Pulmonary embolism (PE) occurs when the pulmonary arteries are obstructed, most often due to emboli from deep veins of thighs/pelvis; together with deep vein thrombosis (DVT), they comprise venous thromboembolism (VTE).
2. Epidemiology: PE is a leading cause of cardiovascular-related death.
3. Pathophysiologic Sequence: Clot forms in deep vein → fragment breaks off → travels through venous system → right heart → pulmonary arteries → obstructs blood flow → impaired gas exchange and hemodynamics.
 4. Nonthrombotic Emboli: Air, fat, amniotic fluid, bacterial (septic), foreign bodies, and tumors can also cause PE.
5. Key Complications: Pulmonary hypertension, right heart failure, and pulmonary infarction.
4. Nonthrombotic Emboli: Air, fat, amniotic fluid, bacterial (septic), foreign bodies, and tumors can also cause PE.
5. Key Complications: Pulmonary hypertension, right heart failure, and pulmonary infarction.
Risk Factors & Assessment
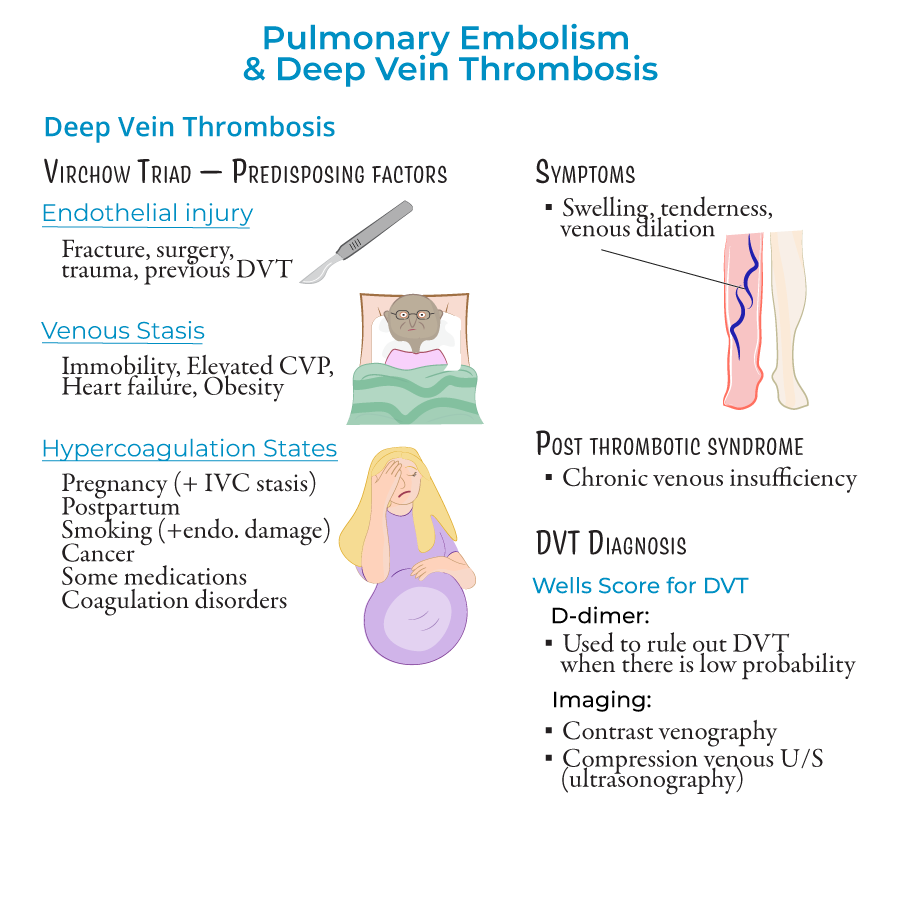
1. Virchow's Triad: Three components predisposing to thrombosis:
- Endothelial injury: Fracture, surgery, trauma, previous DVT; triggers clotting cascade
- Venous stasis: Immobility, elevated central venous pressure, heart failure, obesity
- Hypercoagulable states: Pregnancy and postpartum period, smoking, cancer, hormonal medications, coagulation disorders (Factor V Leiden)
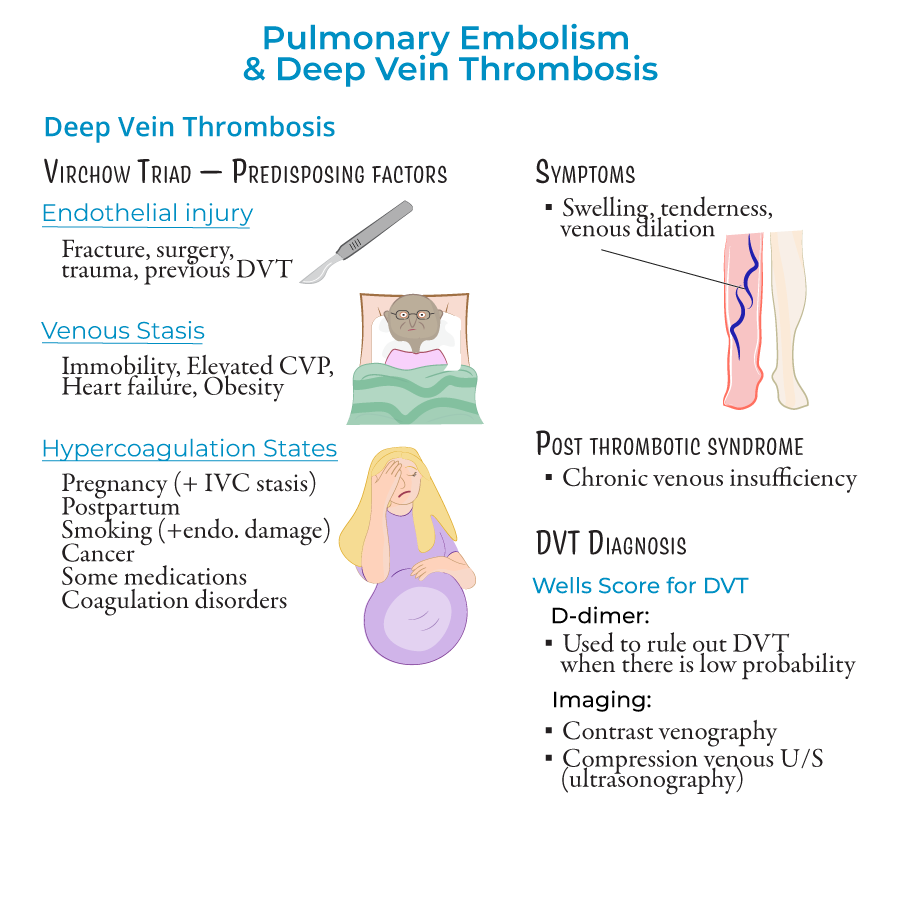 2. Combined Risk Assessment: Patients with multiple predisposing factors have significantly higher risk (e.g., pregnant women on bed rest).
3. Risk Stratification for PE:
2. Combined Risk Assessment: Patients with multiple predisposing factors have significantly higher risk (e.g., pregnant women on bed rest).
3. Risk Stratification for PE:
- Massive (High Risk): Hemodynamically unstable with hypotension
- Intermediate (Submassive): Stable but with evidence of right ventricular dysfunction
- Low Risk: Hemodynamically stable without evidence of right ventricular dysfunction
- Saddle emboli: Located at pulmonary trunk bifurcation
- Lobar, segmental, subsegmental: Located in respective arterial branches
Clinical Presentation & Evaluation
1. DVT Manifestations: Unilateral leg swelling, tenderness, venous dilation; can occur in upper body (less common); post-thrombotic syndrome if venous valves are damaged.
2. PE Symptoms & Signs:
- Dyspnea and tachypnea (rapid breathing)
- Chest pain
- Hypoxemia and ventilation-perfusion mismatch
- Respiratory alkalosis
- Tachycardia and potential right heart failure
- Altered mental state, especially important to recognize in elderly patients
- Wells Score for PE: ≥4 indicates PE likely; <2 low probability, 2-6 moderate, >6 high probability
- Wells Score for DVT: Based on swelling, edema, likelihood of alternative diagnosis
Diagnostic Approach
1. Laboratory Studies:
- D-dimer: >500 ng/mL suggests possible PE/DVT requiring further testing; useful to rule out low-probability cases
- Arterial blood gases: May show hypoxemia and respiratory alkalosis
- CT angiography: Most widely used; visualizes disruption of blood flow in pulmonary arteries
- Ventilation-perfusion scan: Non-invasive test indicating blood clot presence
- Chest X-ray: May show atelectasis, Hampton hump (pulmonary infarction), Westermark sign (oligemic areas), pleural effusion
- Venous ultrasonography with compression: Verifies thrombus presence
- Contrast venography: Alternative method
- Sinus tachycardia
- S1Q3T3 pattern (S wave in lead I, inverted Q and T waves in lead III)
Management & Treatment
1. Supportive Therapy:
- Oxygen administration when saturation <90%
- Saline for fluid management
- Vasopressors if hemodynamically unstable
- Short-term: Heparin, enoxaparin, or fondaparinux
- Long-term: Warfarin
- Monitoring: For efficacy and complications, including heparin-induced thrombocytopenia
- Embolectomy for mechanical removal of clot
- Clot dissolution (thrombolytics) to restore pulmonary arterial flow
- Mechanical: Sequential compression devices (SCDs) to prevent venous stasis
- Pharmacologic: Low-dose enoxaparin or heparin
- --
HIGH YIELD
Clinical Decision-Making Pearls
1. Diagnostic Strategy: Integration of clinical probability assessment, D-dimer testing, and appropriate imaging selection.
2. Risk Assessment Integration: Using both Virchow's Triad elements and PE severity classification to guide management.
3. Recognition of Atypical Presentations: Altered mental status in elderly with PE; upper extremity DVT.
4. Appropriate Threshold for Testing: Balancing overtesting against missed diagnosis based on risk stratification.
5. Differential Diagnosis Refinement: Distinguishing PE from other causes of acute dyspnea and chest pain.
Diagnostic Test Selection & Interpretation
1. D-dimer Utilization: High sensitivity but low specificity; most useful to rule out VTE in low-probability patients.
2. Imaging Selection Logic:
- CT angiography as first-line imaging for suspected PE
- Venous ultrasonography with compression for suspected DVT
- Hampton Hump: Wedge-shaped opacity indicating pulmonary infarction, typically in lower lobes
- Westermark Sign: Focal oligemia appearing as area of poor perfusion
Treatment Decision Points
1. Anticoagulation Initiation: When to start therapy based on clinical suspicion before confirmatory testing.
2. Management Based on PE Classification:
- Massive PE: Considering thrombolytics or embolectomy
- Submassive PE: Anticoagulation with consideration of advanced interventions if deterioration
- Low-risk PE: Anticoagulation alone, possible outpatient management
Virchow's Triad Clinical Applications
1. Endothelial Injury Assessment: Evaluation of recent surgery, trauma, or prior DVT as risk factors.
2. Venous Stasis Identification:
- Immobility risk in hospitalized patients
- Heart failure contribution to reduced flow
- Obesity increasing intra-abdominal pressure
- Pregnancy and postpartum risk periods
- Cancer-associated hypercoagulability
- Medication effects (hormonal contraceptives/therapies)
- Recognition of coagulation disorders
Management of Complications
1. Pulmonary Infarction: Recognition of small emboli causing tissue ischemia; Hampton Hump on X-ray.
2. Right Heart Failure: Assessment and management of increased right ventricular afterload.
3. Heparin-Induced Thrombocytopenia: Monitoring platelet counts; recognition and management of this paradoxical complication.
4. Post-thrombotic Syndrome: Long-term complication of DVT due to venous valve damage.
5. Recurrent VTE: Assessment for underlying hypercoagulable conditions or inadequate anticoagulation.
- --
Beyond the Tutorial
Advanced Management Considerations
1. Anticoagulation Selection: Direct oral anticoagulants (DOACs) vs. warfarin vs. low molecular weight heparin based on patient factors.
2. Extended Anticoagulation: Decision-making for duration based on risk factors for recurrence.
3. Thrombolytic Therapy: Specific indications, contraindications, and administration protocols.
4. Inferior Vena Cava Filters: Indications, placement timing, retrieval considerations.
5. Management of Anticoagulation Complications: Approaches to bleeding events and reversal strategies.
Special Population Management
1. Cancer-Associated Thrombosis: Preferred anticoagulants and duration of therapy.
2. Pregnancy-Related VTE: Anticoagulation selection and monitoring during pregnancy and postpartum.
3. Elderly Patients: Balancing bleeding and thrombotic risks, dose adjustments.
4. Renal Impairment: Anticoagulant selection and dose modifications.
5. Thrombophilia: Testing indications and management implications.
Evidence-Based Preventive Strategies
1. Risk Assessment Models: PADUA, Caprini, and IMPROVE scores for hospitalized patients.
2. Extended Prophylaxis: Indications for continuing prophylaxis post-discharge.
3. Mechanical vs. Pharmacologic Methods: Comparative effectiveness and combination approaches.
4. Special Surgical Populations: Orthopedic, bariatric, neurosurgical prophylaxis considerations.
5. Travel-Related Thrombosis: Evidence-based recommendations for long-distance travelers.
Chronic Thromboembolic Disease
1. Post-PE Syndrome: Chronic dyspnea and functional limitations after PE.
2. Chronic Thromboembolic Pulmonary Hypertension (CTEPH): Diagnostic approach and treatment options.
3. Post-Thrombotic Syndrome Management: Compression therapy and other interventions.
4. Quality of Life Assessment: Functional capacity evaluation and rehabilitation approaches.
5. Long-Term Surveillance: Monitoring for development of chronic complications.
Quality Measures & Systems-Based Practice
1. VTE Prophylaxis Protocols: Hospital-based implementation strategies.
2. Care Transitions: Anticoagulation management across healthcare settings.
3. Quality Metrics: Hospital-acquired VTE rates as healthcare quality indicator.
4. Cost-Effective Diagnostic Strategies: Appropriate use criteria for imaging.
5. Interdisciplinary Management: Collaboration with interventional radiology, vascular medicine, and hematology.
