ABIM - Nausea, Vomiting, Diarrhea
Start your One-Week Free Trial
Already subscribed? Log in »
Here are key facts for ABIM from the Nausea, Vomiting, Diarrhea tutorial, as well as points of interest at the end of this document that are not directly addressed in this tutorial but should help you prepare for the boards. See the tutorial notes for further details and relevant links.
 Below is information not explicitly contained within the tutorial but important for ABIM.
Below is information not explicitly contained within the tutorial but important for ABIM.
- --
VITAL FOR ABIM
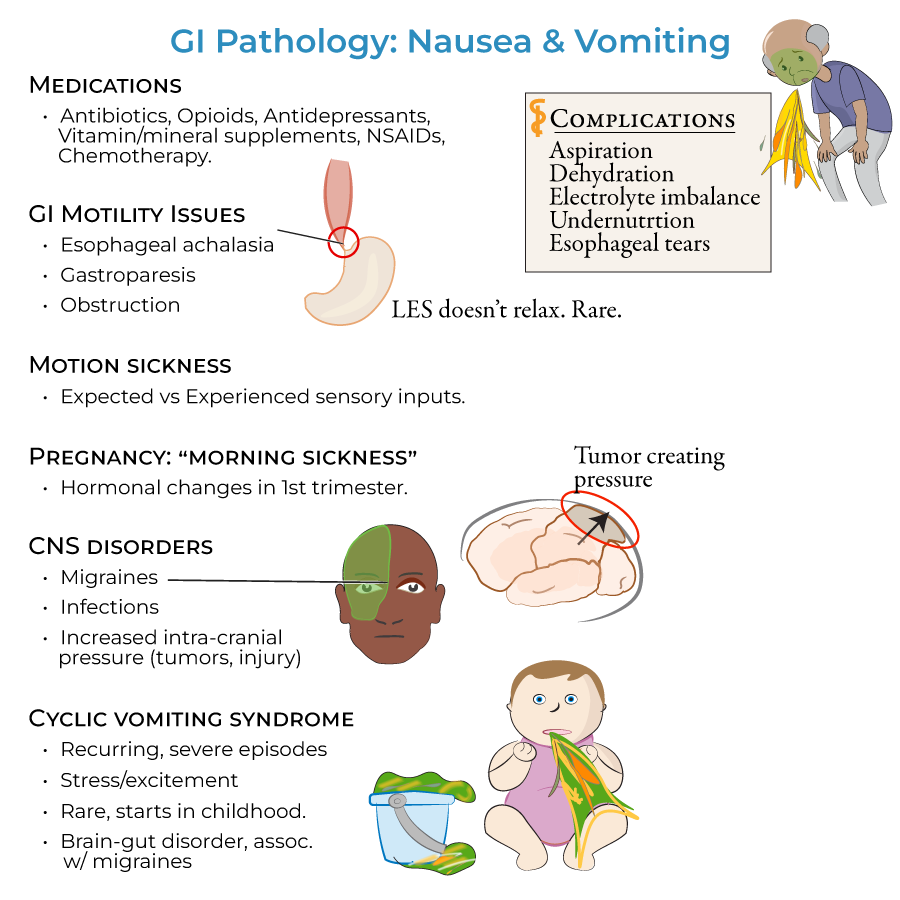
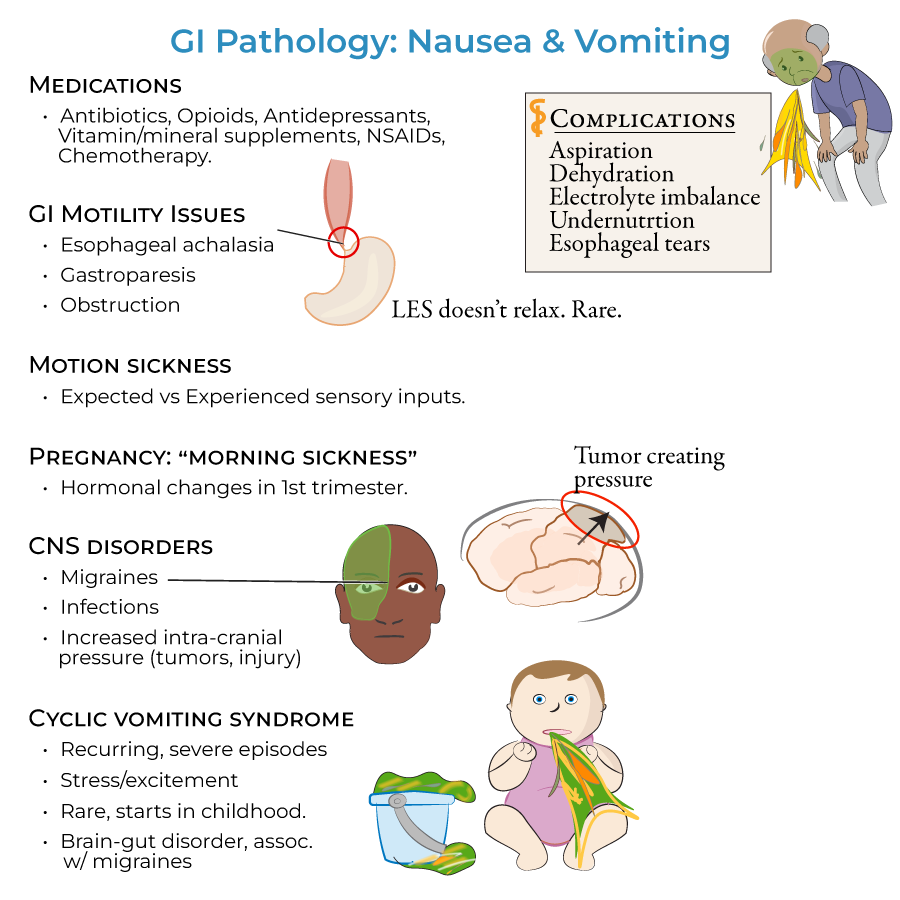
Pathophysiologic Mechanisms
1. Vomiting mechanism: Forceful eviction of the stomach contents caused by contractions of the GI tract and muscles of the thorax
2. Regurgitation mechanism: Ejection of food from the esophagus, distinct from vomiting
3. GI motility disorders: Damaged nerves or mechanical obstruction preventing normal passage of food
Differential Diagnosis - Nausea and Vomiting
1. Medication-induced: Antibiotics, opioids, antidepressants, vitamins and mineral supplements, NSAIDs, chemotherapy
2. Structural causes: Mechanical GI obstructions including adhesions, volvulus, foreign bodies, hernias, tumors
3. Neurological etiologies: Central nervous disorders including migraines, infections, increased intra-cranial pressure
4. Motility disorders: Esophageal achalasia with sustained sphincter contraction, gastroparesis from vagus nerve damage
Differential Diagnosis - Diarrhea
1. Malabsorptive disorders: Lactose intolerance, celiac disease, pancreatic insufficiency
2. Inflammatory conditions: Inflammatory bowel disease (Crohn's disease, ulcerative colitis), microscopic colitis
3. Neoplastic causes: Neuroendocrine tumors producing carcinoid syndrome
4. Combined syndromes: Intestinal ischemia when mesenteric arteries become blocked
Complications and Sequelae
1. Vomiting complications: Aspiration, dehydration, electrolyte imbalance, undernutrition, and esophageal tears
2. Diarrhea complications: Malabsorption of nutrients, dehydration, and electrolyte imbalances
- --
HIGH YIELD
Specific Clinical Entities
1. Esophageal achalasia: Damaged esophageal nerves causing sustained lower esophageal sphincter contraction, presenting with heartburn, chest pain, and regurgitation
2. Gastroparesis: Vagus nerve damage and loss of stomach muscle function leading to early satiety, heartburn and vomiting
3. Cyclical vomiting syndrome: Recurring severe episodes triggered by stress and excitement, thought to result from disordered brain-gut interactions
Diagnostic Pearls
1. Pancreatic insufficiency: Characterized by steatorrhea with oily, foul smelling, yellowish stools that float due to high fat content
2. IBD differentiation: Crohn's disease presents with mucous diarrhea while ulcerative colitis presents with bloody diarrhea
3. Carcinoid syndrome: Found in 30-40% of neuroendocrine tumor patients, presenting with watery, loose stools, flushing, wheezing, and valvular heart disease
Multisystem Involvement
1. Vascular presentations: Intestinal ischemia causing the triad of nausea, vomiting and bloody diarrhea
2. Functional disorders: Irritable bowel syndrome resulting from disordered brain-gut communication
3. Endocrine manifestations: Thyroid disorders, adrenal insufficiency, and diabetes presenting with GI symptoms
Challenging Clinical Scenarios
1. Motion sickness: Results from mismatch between expected and experienced sensory inputs
2. Infectious gastroenteritis: Caused by norovirus, rotavirus, E. coli, Salmonella, Shigella, and Campylobacter
3. Inflammatory conditions: Microscopic colitis presenting with watery diarrhea
- --
Beyond the Tutorial
Advanced Diagnostic Approach
1. Biomarkers: Role of fecal calprotectin, lactoferrin, and pancreatic elastase
2. Endoscopic evaluation: Indications for upper endoscopy, colonoscopy, and capsule endoscopy
3. Functional testing: Gastric emptying studies, manometry, and breath tests
Evidence-Based Management
1. Antiemetic therapy: Agent selection based on receptor involvement and underlying cause
2. Antidiarrheal approaches: Risk-benefit assessment and contraindications
3. Disease-modifying therapies: Immunomodulators and biologics for inflammatory conditions
Complex Case Management
1. Refractory symptoms: Diagnostic algorithm and therapeutic escalation
2. Overlap syndromes: Management of concurrent functional and organic pathologies
3. Nutritional support: Indications and approaches for enteral and parenteral nutrition
System-Based Practice
1. Quality metrics: Reducing hospital readmissions and complications
2. Cost-effective care: Appropriate use of diagnostic testing and therapeutic interventions
3. Multidisciplinary approach: Integration of gastroenterology, surgery, and nutrition services
