ABIM - Liver Disease Overview
Start your One-Week Free Trial
Already subscribed? Log in »
Here are key facts for ABIM from the Liver Pathophysiology Overview tutorial, as well as points of interest at the end of this document that are not directly addressed in this tutorial but should help you prepare for the boards. See the tutorial notes for further details and relevant links.
 Below is information not explicitly contained within the tutorial but important for ABIM.
Below is information not explicitly contained within the tutorial but important for ABIM.
- --
VITAL FOR ABIM
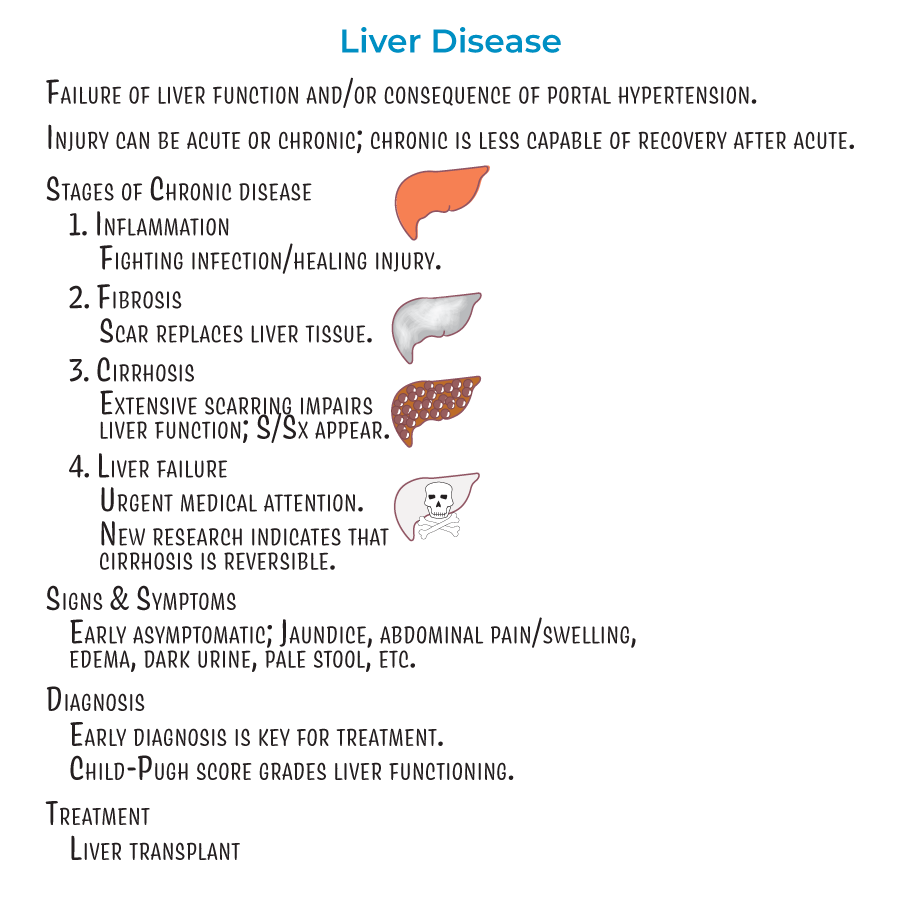
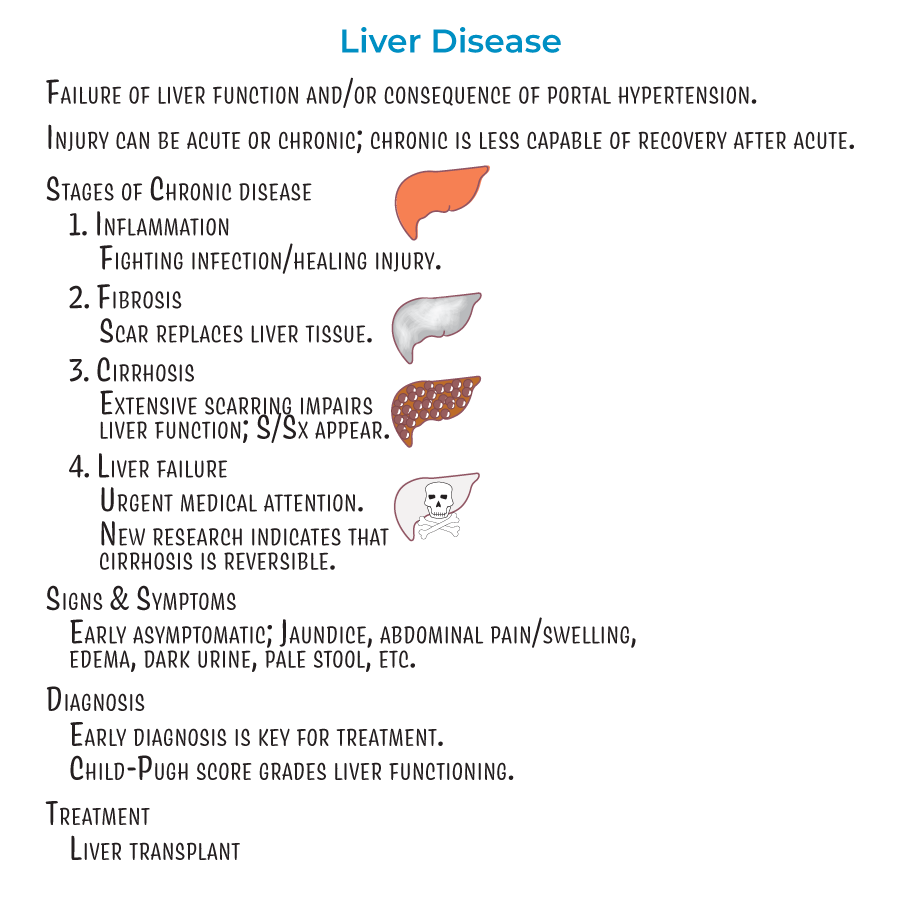
Liver Disease Progression
1. Progressive Stages: Liver disease advances through inflammation (Stage 1), fibrosis (Stage 2), cirrhosis (Stage 3), and liver failure (Stage 4).
2. Pathophysiological Continuum: Injury can be acute, or it can be chronic. A liver undergoing chronic damage is less capable of recovery from acute injury.
3. Recovery Potential: Newer research indicates that cirrhosis (stage 3) is also reversible, not just stages 1 and 2.
4. Clinical Assessment: The Child-Pugh score is used to grade liver functioning.
5. Definitive Management: In cases of cirrhosis or failure, transplants may be the best option.
Liver Functions and Pathophysiology
1. Metabolic Roles: Energy metabolism – the liver plays key roles in carbohydrate and lipid metabolism.
2. Protein Synthesis: Plasma protein synthesis – albumin and other binding proteins, clotting factors, angiotensinogen, IGF-1 and other proteins are synthesized by the liver.
3. Nutrient Storage: Storage – glucose, vitamins B12, D, and K, copper, and iron are stored by the liver.
4. Detoxification: Degradation, detoxification, and clearance – the liver breaks down and/or clears several substances, including ammonia (to form urea), bilirubin, drugs, and other toxins.
Etiologies of Liver Disease
1. Infectious Causes: Infections, such as viral hepatitis and Schistosomiasis.
2. Metabolic Disorders: Fatty liver disease, including alcoholic and nonalcoholic forms.
3. Genetic Conditions: Genetics and hereditary disorders, such as hereditary hemochromatosis.
4. Autoimmune Process: Autoimmune hepatitis.
5. Biliary Pathologies: Biliary tract diseases, such as primary sclerosing cholangitis, primary biliary cholangitis, and secondary biliary cholangitis.
Cirrhosis and Portal Hypertension
1. Structural Changes: Cirrhosis is characterized by the presence of fibrosis and regenerative nodules with fatty changes.
2. Vascular Pathophysiology: Portal hypertension is increased hepatic blood pressure (above 6 mmHg).

- --
HIGH YIELD
Complications of Impaired Hepatic Function
1. Coagulation Abnormalities: Coagulopathy results from decreased storage of vitamin K and synthesis of clotting factors.
2. Neurological Manifestations: Hepatic encephalopathy is the result of toxin build-up in the blood; ammonia is thought to be a key culprit.
3. Clinical Sign: Asterixis, aka, "flapping hand tremor" or "liver flap" is the inability for a patient to sustain a posture due to involuntary, brief, "shock-like" movements.
4. Endocrine Effects: Elevated estrogen levels can cause spider angiomas, palmar erythema, and gynecomastia.
5. Metabolic Derangements: Glucose metabolism is dynamically altered in liver damage so that patients can be hyper- or hypoglycemic.
Portal Hypertension Sequelae
1. Variceal Development: Varices are collateral blood vessels that form to provide alternative blood flow routes; pose significant risk for hemorrhage and are an important cause of GI bleeding.
2. Ascites Formation: Ascites refers to the accumulation of fluid in the peritoneum caused by systemic dilation that allows fluid leakage.
3. Bacterial Peritonitis: Spontaneous Bacterial Peritonitis (SBP) is an acute infection resulting from bacteria and endotoxins leaking from the GI tract, and can lead to septic shock if not treated promptly.
4. Renal Dysfunction: Renal insufficiency and failure are the result of local vasoconstriction and inflammatory processes that reduce filtration.
5. SBP-Renal Connection: Spontaneous bacterial peritonitis is often a trigger for renal failure, as it induces the release of pro-inflammatory molecules that contribute to renal dysfunction.
6. Pulmonary Complications: Hepatopulmonary syndrome, in which pulmonary vasodilation leads to a ventilation/perfusion mismatch, reduced oxygenation, and hypoxemia.
7. Oncologic Risk: Increased risk of liver cancer.
Additional Complications
1. Nutritional Effects: Impaired bile flow can lead to hyperlipidemia, jaundice, and malabsorption of GI contents.
- --
Beyond the Tutorial
Advanced Diagnostic Approaches
1. Laboratory Interpretation: Patterns of liver enzyme elevation (hepatocellular vs. cholestatic), synthetic function assessment (albumin, INR), and specialized testing (ceruloplasmin, alpha-1 antitrypsin, auto-antibodies).
2. Imaging Modalities: Transient elastography (FibroScan) for fibrosis assessment, contrast-enhanced ultrasound for lesion characterization, MR elastography for comprehensive fibrosis staging.
3. Endoscopic Evaluation: Endoscopic retrograde cholangiopancreatography (ERCP) for biliary disease, endoscopic ultrasound (EUS) for lesion assessment and staging.
4. Prognostic Scoring: MELD-Na score for transplant prioritization, CLIF-SOFA for acute-on-chronic liver failure, Lille score for alcoholic hepatitis.
Management Principles
1. Ascites Treatment Algorithm: First-line (sodium restriction, spironolactone), second-line (add furosemide, titrate doses), refractory management (large volume paracentesis with albumin, TIPS evaluation).
2. Variceal Bleeding Protocol: Hemodynamic stabilization, antibiotic prophylaxis, vasoactive drugs (octreotide, terlipressin), endoscopic therapy (band ligation preferred over sclerotherapy), early TIPS for high-risk patients.
3. Hepatorenal Syndrome: Vasoconstrictors (norepinephrine, terlipressin) with albumin, avoidance of nephrotoxins, renal replacement therapy considerations.
4. Encephalopathy Management: Lactulose (titrated to 2-3 soft bowel movements daily), rifaximin for recurrent episodes, investigation of precipitating factors, ammonia-lowering strategies.
Special Populations
1. Acute-on-Chronic Liver Failure: Recognition of rapid decompensation, multiorgan support, prognostic assessment, transplant considerations.
2. Alcoholic Hepatitis: Maddrey's discriminant function calculation, steroid therapy indications, pentoxifylline alternatives, liver transplant controversies.
3. Pregnancy Considerations: Differential diagnosis of liver disease unique to pregnancy (HELLP, acute fatty liver, intrahepatic cholestasis), management adaptations.
4. Older Adults: Medication dosing adjustments, falls risk assessment, nutritional optimization, cognitive evaluation.
Emerging Concepts
1. Microbiome Manipulation: Probiotics, fecal microbiota transplantation, and targeted antibiotics for various liver disease manifestations.
2. Antifibrotic Therapies: Novel agents targeting hepatic stellate cell activation, collagen deposition, and fibrogenesis.
3. Artificial Liver Support: Bioartificial systems, albumin dialysis (MARS), and molecular adsorbent recirculating systems as bridges to recovery or transplantation.
4. Precision Medicine: Genotype-directed therapy for specific liver diseases, pharmacogenomics for drug metabolism optimization.
