ABIM - Large Vessel Vasculitis
Start your One-Week Free Trial
Already subscribed? Log in »
Here are key facts for ABIM from the Large Vessel Vasculitis tutorial, as well as points of interest at the end of this document that are not directly addressed in this tutorial but should help you prepare for the boards. See the tutorial notes for further details and relevant links.
- --
VITAL FOR ABIM
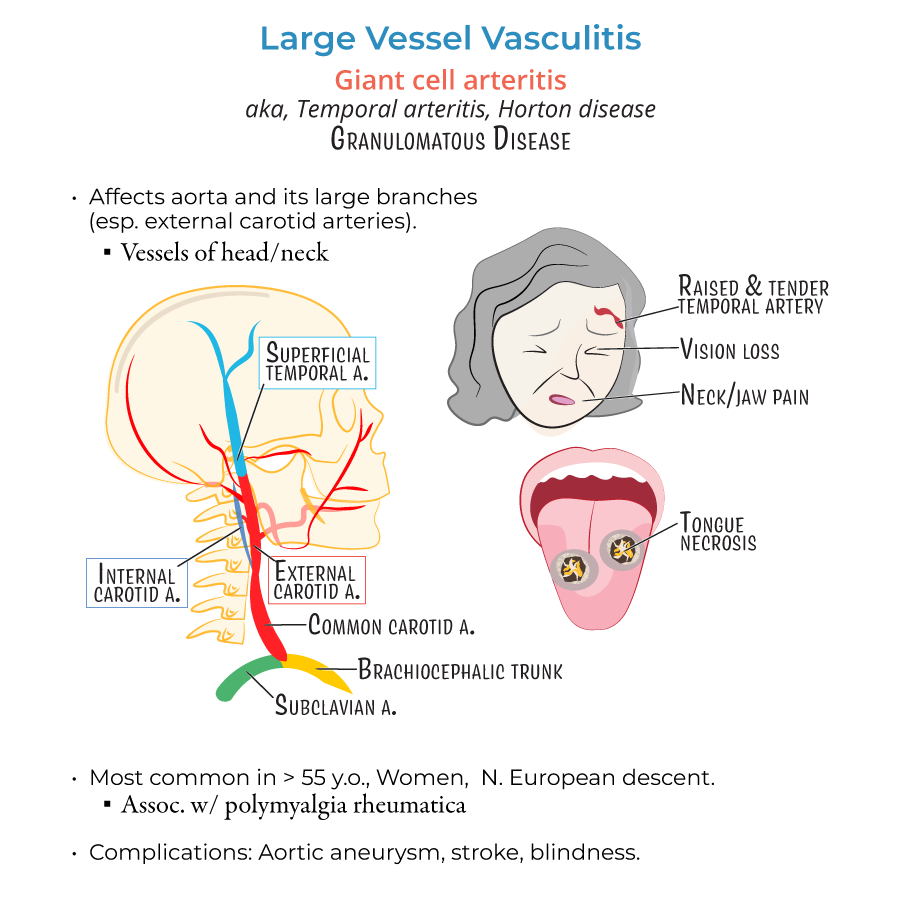
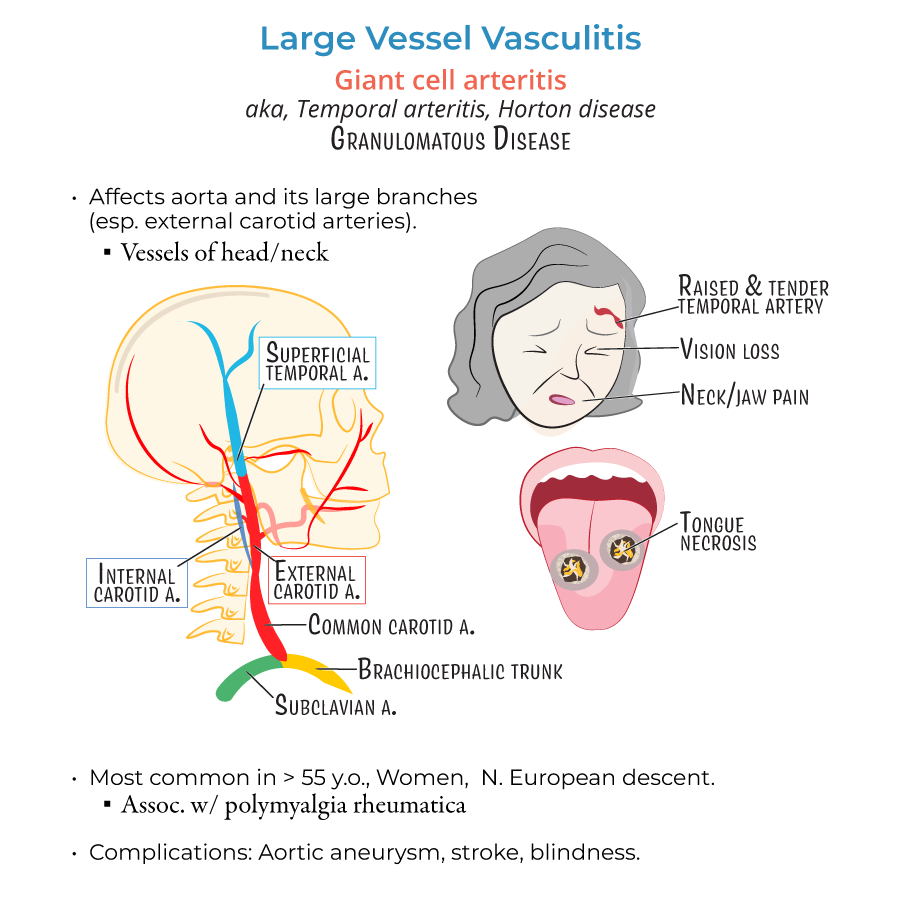
Giant Cell Arteritis (GCA)
1. GCA affects large vessels, particularly the branches of the external carotid artery, such as the temporal artery.
2. Typical demographic: women over 50 years old, especially of Northern European descent.
3. Clinical presentation:
- New-onset temporal headache
- Jaw claudication (pain when chewing)
- Scalp tenderness
- Visual symptoms (amaurosis fugax, blurred vision, possible permanent blindness)
- Polymyalgia rheumatica association (proximal muscle pain and stiffness)
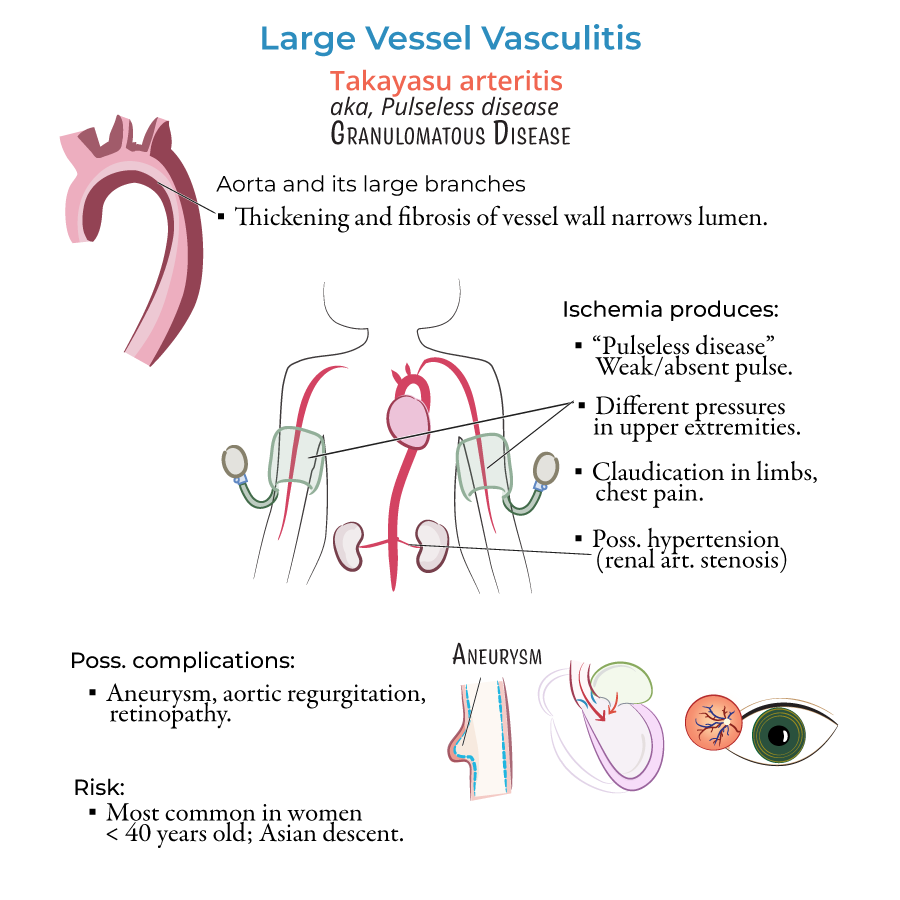
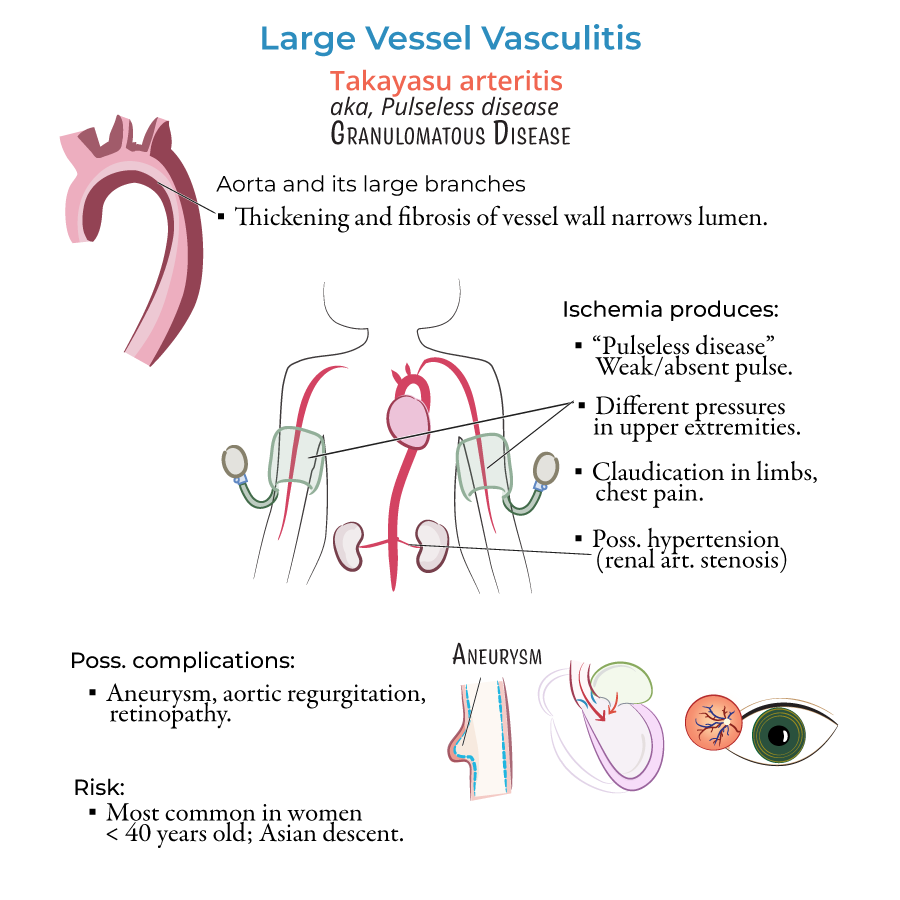
Takayasu Arteritis
8. Takayasu arteritis involves granulomatous inflammation of the aorta and its major branches.
9. Typical demographic: young women (<40 years), especially of Asian descent.
10. Clinical presentation:
- Decreased or absent pulses (e.g., brachial, radial)
- Blood pressure difference between arms (>10 mmHg)
- Arm or leg claudication
- Bruits over subclavian or carotid arteries
- Hypertension (due to renal artery involvement)
- --
HIGH YIELD
Pathophysiology and Histology
1. Both GCA and Takayasu are granulomatous vasculitides targeting large vessels.
2. Histologic findings include:
- Granulomatous inflammation
- Multinucleated giant cells
- Destruction of the internal elastic lamina
- Intimal hyperplasia leading to luminal narrowing
Diagnostic and Laboratory Evaluation
4. Temporal artery biopsy is gold standard for GCA but may have patchy involvement (false negatives possible).
5. Elevated ESR (>50 mm/hr) and CRP are nonspecific but strongly supportive.
6. Anemia of chronic disease may be present in both conditions.
7. Imaging for Takayasu should evaluate the full aorta and major branches (CT/MRI).
Management and Monitoring
8. In GCA:
- Start corticosteroids immediately.
- If visual symptoms occur, hospitalize for IV methylprednisolone.
- Use systemic corticosteroids initially.
- Methotrexate or azathioprine may be used as steroid-sparing agents.
- --
Beyond the Tutorial
Long-Term Management and Complications
1. For GCA:
- Steroid taper guided by symptoms and inflammatory markers.
- Low-dose aspirin is often recommended to reduce stroke risk.
- Monitor for aortic aneurysm development (especially thoracic).
- Monitor for development of aortic aneurysms, renal artery stenosis, and aortic regurgitation.
- Annual imaging may be needed to detect progression.
- Antihypertensive therapy is often required if renal arteries are involved.
Medication Side Effects and Prevention
3. Chronic steroid use requires:
- Bone protection (calcium, vitamin D, bisphosphonates)
- Monitoring for hyperglycemia, infections, and myopathy
