ABIM - Ischemic Heart Disease Pathophysiology
Start your One-Week Free Trial
Already subscribed? Log in »
Here are key facts for ABIM Certification Examination from the Ischemic Heart Disease tutorial, focusing on evidence-based management, diagnostic approaches, and current clinical understanding, as well as points of interest at the end that are not directly addressed in this tutorial but should help you prepare for the boards. See the tutorial notes for further details and relevant links.
 Below is additional information important for ABIM Certification not explicitly contained within the tutorial.
Below is additional information important for ABIM Certification not explicitly contained within the tutorial.
- --
- --
VITAL FOR ABIM
Cardiac Ischemia: Basic Concepts
1. Definition: Cardiac ischemia occurs when coronary blood flow doesn't keep up with the metabolic needs of the heart.
2. Result: Mechanical and/or electrical functions are impaired.
3. Causes:
- Extravascular events (increased intramyocardial pressure, reduced diastolic filling time)
- Coronary vascular dysfunction
Epidemiology and Risk Factors
1. Prevalence: Ischemic heart disease is the leading cause of death in both men and women.
2. Disparities: Sex and racial differences in pathology and symptoms may delay diagnosis and treatment.
3. Risk factors:
- Family history, increasing age, smoking, hypertension, diabetes, hyperlipidemia, obesity
- Low physical activity levels, early menopause
- Gestational diabetes and gestational hypertension
- Chronic inflammatory rheumatoid diseases
- Several are related to metabolic and/or inflammatory conditions
- Studies suggest many are stronger risk factors in women than men
Pathophysiologic Classification
1. Obstructive Coronary Artery Disease:
- Atherosclerotic plaques obstruct ≥50% of epicardial artery lumen
- Primarily seen in men >45 years of age; women >55 years at elevated risk
- Plaques can rupture or erode, producing thrombi leading to acute coronary events
- Key insight: Up to half of patients who undergo angiogram have no significant coronary obstruction
- Smaller plaques blocking <50% of lumen without significant obstruction
- Particularly common in women; present in ~30% of men
- Associated with elevated risk of Major Adverse Cardiovascular Events (MACE), particularly in younger women
- May involve plaque erosion, microvascular disease and/or vasospasm
- --
HIGH YIELD
Coronary Blood Supply
1. Epicardial coronary arteries: Run along heart surface (left and right coronary arteries and branches).
2. Microvasculature: Prearterioles, arterioles, and capillaries in deeper cardiac tissues.
3. Functional role: Prearterioles and arterioles provide resistance and regulation of blood flow.
Plaque Rupture vs. Erosion
1. Plaque rupture:
- Occurs when tears in fibrous caps release thrombogenic contents into vessel lumen
- Characterized by lipid cores, thin caps, producing fibrin-rich "red thrombi"
- Historically important cause of thrombus and ischemia
- Less often implicated in acute coronary syndrome due to reduced atherosclerosis from statins and other drugs
- Increasingly significant cause of acute coronary syndrome
- More common in women, young individuals, smokers, and diabetics
- Occurs when a plaque with thick cap produces a platelet-rich white thrombus
- Associated with fractured or absent vessel endothelium, suggesting dysfunctional endothelium
Coronary Microvascular Dysfunction
1. Clinical significance:
- Significant cause of INOCA, though can coexist with Obstructive CAD
- Associated with elevated risk of Major Adverse Cardiovascular Events
- Recent studies show it affects both sexes in near-equal proportions
- Structural: Arteriole remodeling producing thicker medial and intimal walls, reduced wall:lumen ratio
- Functional: Impaired vasodilation due to endothelial dysfunction and/or other causes, vasospasms
- Pattern: Diffuse in myocardium, producing patchy areas of ischemia (vs. localized lesions of epicardial obstruction)
- Extravascular mechanisms: Can impair coronary microcirculation
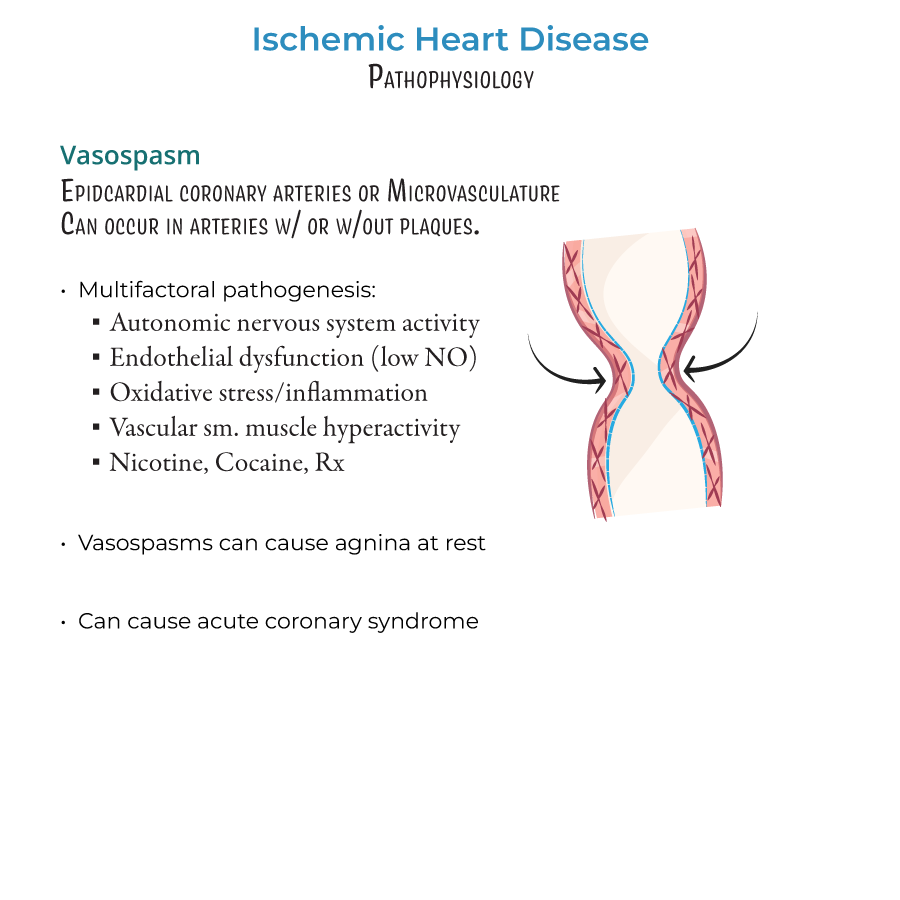
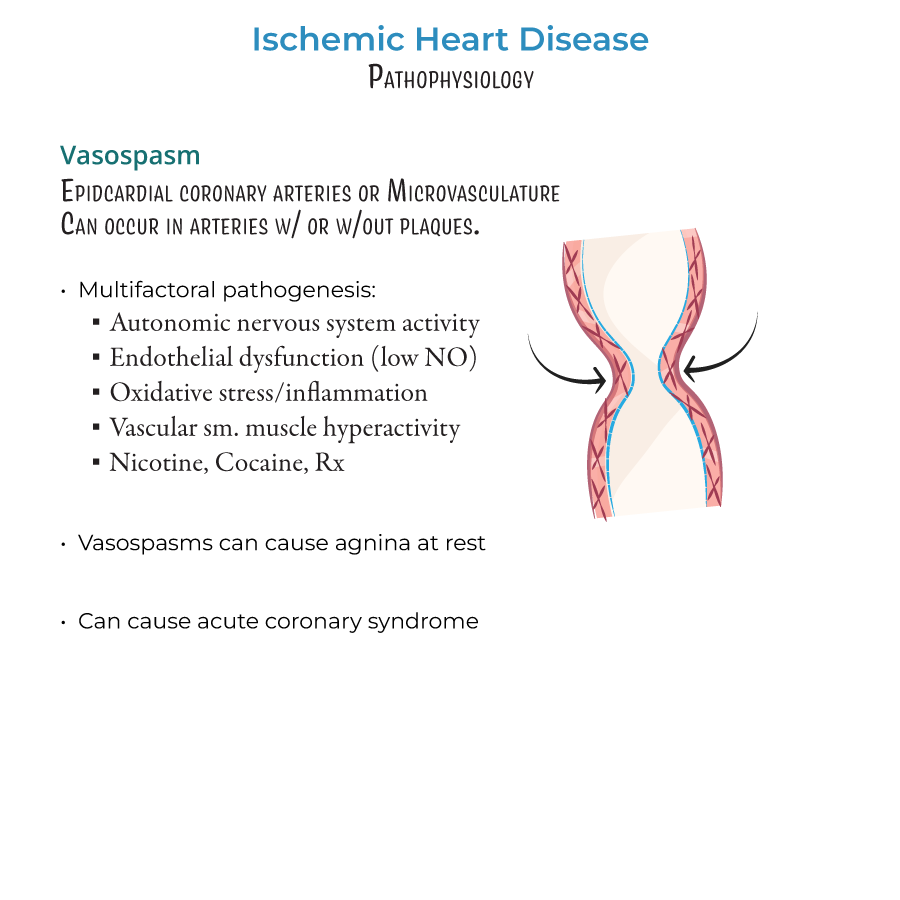
Vasospasm
1. Location: Occur in epicardial coronary arteries and microvasculature.
2. Context: Occur in presence or absence of stenosis.
3. Mechanisms/triggers:
- Enhanced autonomic nervous system activity
- Endothelial dysfunction (especially reduced nitric oxide)
- Oxidative stress and inflammation causing damage and constriction
- Vascular smooth muscle hyperactivity
- Substances: nicotine, cocaine, vasoconstricting medications
- --
Beyond the Tutorial
Diagnostic Approach and Evaluation
1. Non-invasive testing strategies:
- Exercise ECG testing: Sensitivity ~68%, specificity ~77%
- Stress echocardiography: Sensitivity ~80-85%, specificity ~80-88%
- Nuclear myocardial perfusion imaging: Sensitivity ~85-90%, specificity ~70-75%
- Coronary CT angiography: High NPV for excluding CAD, limited for functional assessment
- Cardiac MRI: Excellent for ischemia detection and viability assessment
- Coronary angiography: Gold standard for epicardial CAD assessment
- FFR/iFR: Functional significance of intermediate lesions
- IVUS/OCT: Plaque characterization and stent optimization
- Coronary flow reserve: Microvascular function assessment
- Acetylcholine testing: Vasospasm provocation
- Pre-test probability assessment (Diamond-Forrester, ASCVD risk score)
- CCS/AHA/ACC appropriate use criteria for diagnostic testing
- Risk stratification for stable and unstable patients (TIMI, GRACE, HEART scores)
Evidence-Based Management
1. Acute coronary syndrome:
- Early invasive strategy for high-risk NSTEMI (Class I, LOE A)
- Primary PCI for STEMI within 90 minutes of first medical contact (Class I, LOE A)
- DAPT: Aspirin + P2Y12 inhibitor (Class I, LOE A)
- Duration based on clinical scenario, bleeding risk, stent type
- Beta-blockers, ACE-I/ARB, high-intensity statins (Class I recommendations)
- Optimal medical therapy (OMT) as first-line (Class I, LOE A)
- Revascularization for refractory symptoms or high-risk anatomy
- ISCHEMIA trial insights: Similar outcomes for OMT vs. invasive strategy in stable patients
- Indications for CABG vs. PCI based on SYNTAX score, LM/3VD, diabetes
- Microvascular dysfunction: Beta-blockers, CCBs, ACE-I/ARBs, ranolazine
- Vasospastic angina: CCBs, long-acting nitrates (avoid beta-blockers)
- INOCA: Targeted therapy based on physiologic testing
- Prevention of plaque erosion: Antiplatelet therapy, smoking cessation
Emerging Concepts and Therapies
1. Anti-inflammatory approaches:
- Colchicine: COLCOT and LoDoCo2 trials showing benefit in post-MI patients
- CANTOS trial: IL-1β inhibition
- Targeting inflammation to prevent plaque complications
- PCSK9 inhibitors: FOURIER and ODYSSEY OUTCOMES trials
- Bempedoic acid: ATP citrate lyase inhibition
- RNA-based therapies: Inclisiran (siRNA targeting PCSK9)
- Genetic risk assessment (polygenic risk scores)
- Biomarker-guided therapy
- Sex-specific diagnostic and therapeutic approaches
- Tailored antiplatelet therapy based on bleeding/thrombotic risk
