ABIM - Inflammatory Bowel Disease
Start your One-Week Free Trial
Already subscribed? Log in »
Here are key facts for ABIM from the Inflammatory Bowel Disease tutorial, as well as points of interest at the end of this document that are not directly addressed in this tutorial but should help you prepare for the boards. See the tutorial notes for further details and relevant links.
- --
VITAL FOR ABIM
Inflammatory Bowel Disease (IBD) - Clinical Overview
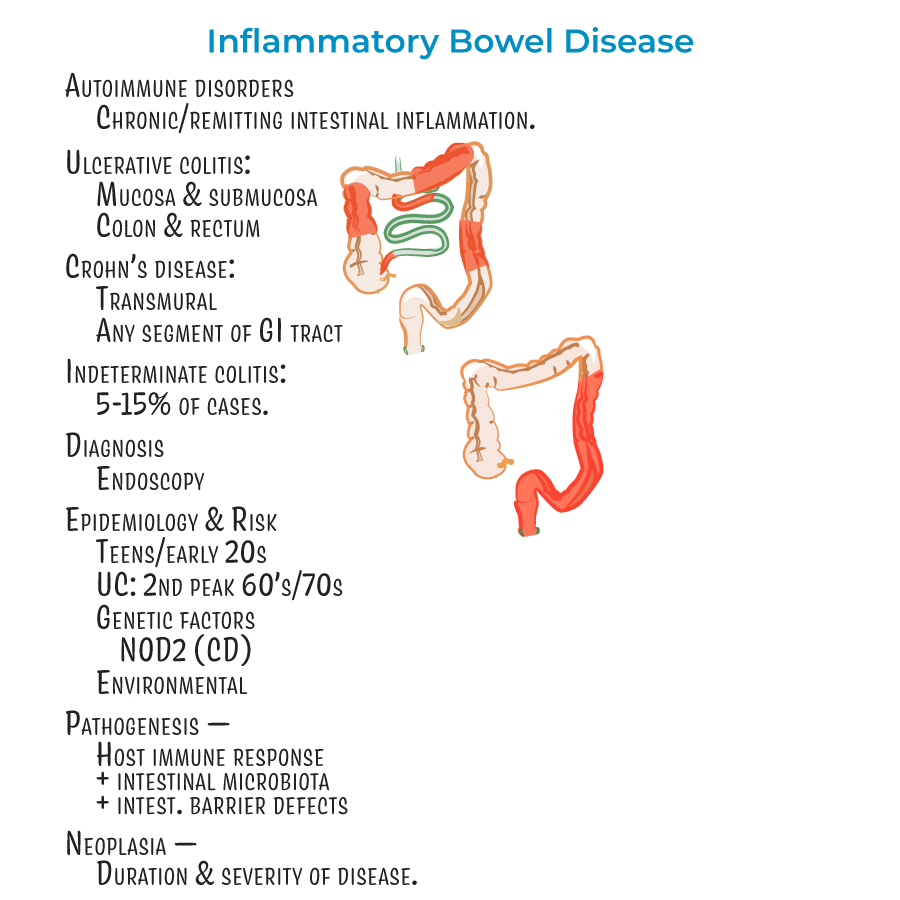
1. Autoimmune disorders characterized by chronic or remitting intestinal inflammation.
2. Diagnosis relies on endoscopy.
3. Demographic pattern: Most patients diagnosed in teens/early 20s; ulcerative colitis has a second "peak" in patients in their 60's or 70's.
4. Associated with neoplasia, with risk influenced by duration and severity of disease.
5. Extraintestinal manifestations: Most common are skin lesions (in up to 40% of patients), uveitis, and arthritis.
6. Less common but potentially deadly complications: involvement of liver/gallbladder, lung, pancreas, and kidneys.
Crohn's Disease - Clinical Features and Management
1. Pathophysiology: Transmural inflammation (can reach all layers of GI tract).
2. Distribution: Can affect any segment of GI tract, but most commonly involves ileum and colon with "skip lesions" (discontinuous pattern).
3. Rectum usually spared (unlike ulcerative colitis).
4. Clinical presentation: Abdominal cramping (often on the right side, where the ileum meets the large intestine), diarrhea (potentially bloody), fever and malaise, weight loss (due to malabsorption), perianal lesions (25% of patients).
5. Complications: Problems related to fistulas, fissures, and obstructive strictures; dysplasia and adenocarcinoma; and anemia from chronic blood loss.
6. Treatment approach: Patients advised to avoid cigarette smoking and nicotine (exacerbates inflammation), anti-inflammatories, immune suppressors, surgery to remove parts of the colon.
Ulcerative Colitis - Clinical Features and Management
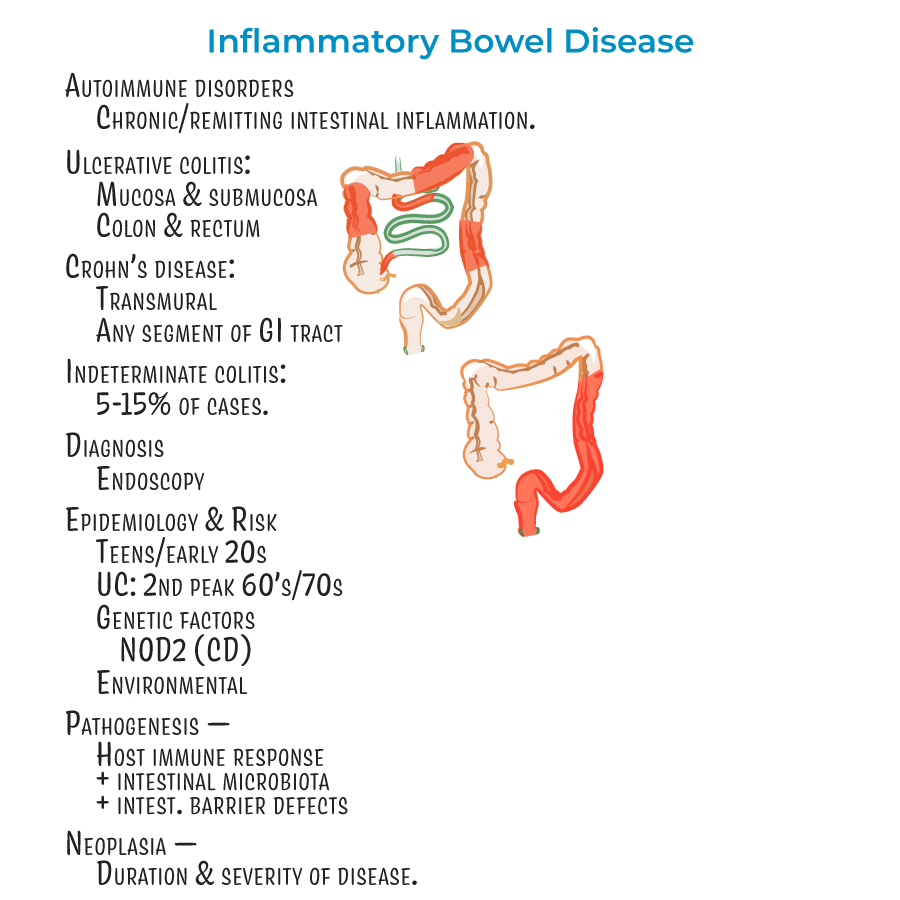
1. Pathophysiology: Inflammation of mucosal and submucosal layers only.
2. Distribution: Restricted to the colon and rectum with continuous lesions.
3. Endoscopic findings: Sunken, red/bloody ulcers with friable appearance; remaining mucosa creates "pseudopolyps."
4. Clinical presentation: Bloody diarrhea with rectal bleeding, abdominal pain, fever, and weight loss.
5. Complications: Toxic ulceritis, toxic megacolon, intestinal perforation. Dysplasia and adenocarcinoma more likely when entire colon is involved (pancolitis).
6. Treatment approach: Anti-inflammatories, immune suppressors, and colectomy. Patients who smoke cigarettes more likely to experience bouts upon quitting.
- --
HIGH YIELD
IBD Pathophysiology and Risk Factors
1. Genetic factors play a role in development (e.g., mutations in NOD2 associated with Crohn's disease).
2. Environmental factors are important in management (diet, cigarette smoking, medications).
3. Result of detrimental interactions between host immune response, intestinal microbiota, and intestinal barrier defects.
4. About 5-15% of cases are considered "indeterminant" colitis when distinction between UC and CD is difficult.
5. Different types of T-helper cells play major roles: Th1/Th17 cell-mediated inflammation in Crohn's disease versus Th2 cell-mediated inflammation in ulcerative colitis.
Crohn's Disease - Diagnostic Features
1. Many studies suggest a female predominance.
2. Transmural inflammation with wall thickening and "creeping fat" that wraps around the GI tract.
3. Progressive lesion morphology:
- Aphthous erosions (early shallow whitish sores)
- Longitudinal "bear claw" ulcers (look like rake dragged down GI lining)
- Cobblestone appearance (as tissue becomes crowded with ulcers)
- Fissures form and progress to fistulas (connecting to abdominal/pelvic cavity or other organs)
Ulcerative Colitis - Diagnostic Features
1. Inflammation destroys submucosal vascular network.
2. Mucosa is bloody during active inflammation.
3. Histology: Branching and distension of intestinal crypts, crypt abscesses with neutrophils.
4. Continuous lesions starting from rectum (unlike Crohn's disease).
Clinical Distinctions for Differential Diagnosis
1. Key differences:
- CD = transmural inflammation, skip lesions, any GI segment, rectum usually spared
- UC = mucosal/submucosal inflammation, continuous lesions, colon/rectum only
- --
Beyond the Tutorial
Advanced Diagnostic Approach
1. Laboratory evaluation:
- Anemia profile: iron studies, B12, folate
- Inflammatory markers: CRP, ESR, fecal calprotectin
- Serology: ASCA (associated with CD), p-ANCA (associated with UC)
- Microbial studies to exclude infectious colitis
- Nutritional parameters: albumin, pre-albumin, vitamin D
- Upper endoscopy for suspected upper GI Crohn's involvement
- Ileocolonoscopy with biopsies (targeted and random)
- Endoscopic scoring systems: Mayo score for UC, SES-CD or CDEIS for Crohn's
- Narrow-band imaging and chromoendoscopy for dysplasia surveillance
- Video capsule endoscopy for small bowel evaluation (contraindicated with strictures)
- CT enterography: protocol and findings interpretation
- MR enterography: advantages in radiation-sensitive populations
- Small bowel follow-through: role in resource-limited settings
- Abdominal ultrasound: emerging role in monitoring disease activity
- Microscopic patterns of chronic vs. acute inflammation
- Architectural distortion patterns
- Granuloma identification and significance
- Dysplasia grading and management implications
Evidence-Based Treatment Algorithms
1. Induction therapy:
- 5-ASA compounds: efficacy in UC vs. limited role in CD
- Corticosteroids: dosing strategies, tapering protocols, steroid-sparing approaches
- Biologics: anti-TNF (infliximab, adalimumab, golimumab, certolizumab)
- Anti-integrin therapy: vedolizumab mechanism and patient selection
- Anti-IL12/23: ustekinumab indications and dosing
- JAK inhibitors: tofacitinib and emerging agents
- Combination therapy vs. monotherapy decision-making
- Risk stratification for aggressive disease
- Therapeutic drug monitoring: reactive vs. proactive approaches
- Immunomodulator optimization: thiopurines, methotrexate
- Biologic dose optimization and interval adjustment
- Duration of therapy considerations
- De-escalation approaches in deep remission
- Primary non-response vs. secondary loss of response
- Within-class vs. out-of-class switching
- Combination therapy intensification
- Clinical trial eligibility assessment
- Surgical timing and patient selection
Management of Complications
1. Acute severe ulcerative colitis:
- Oxford criteria and Truelove-Witts classification
- Inpatient management protocol
- Rescue therapy selection: cyclosporine vs. infliximab
- Predictors of colectomy
- Post-discharge management and prevention of recurrence
- Differentiating inflammatory vs. fibrotic strictures
- Endoscopic balloon dilation technique and outcomes
- Strictureplasty vs. resection decision factors
- Post-operative pharmacological prophylaxis
- Classification systems for perianal disease
- Combined medical-surgical approach
- Role of imaging: MRI, endoanal ultrasound
- Seton placement and management
- Definitive surgical approaches
- Joint involvement: axial vs. peripheral arthropathy management
- Dermatological manifestations: treatment algorithm
- Ocular complications: screening and management
- Primary sclerosing cholangitis: surveillance and management
- Thromboembolic risk assessment and prophylaxis
Special Clinical Scenarios
1. Pregnancy and IBD:
- Pre-conception optimization
- Medication safety by trimester
- Disease monitoring during pregnancy
- Mode of delivery considerations
- Flare management during pregnancy
- Breastfeeding considerations
- Polypharmacy considerations
- Immunosuppression risks
- Modified therapeutic goals
- Quality of life assessment
- Age-appropriate cancer surveillance
- Preoperative optimization
- Medication management perioperatively
- Venous thromboembolism prophylaxis
- Nutritional support
- Ostomy care considerations
- Risk stratification
- Surveillance intervals based on risk profile
- Chromoendoscopy technique
- Management of indefinite vs. low-grade vs. high-grade dysplasia
- Post-colectomy surveillance in Crohn's colitis
