ABIM - Hypertension Pathophysiology
Start your One-Week Free Trial
Already subscribed? Log in »
Here are key facts for American Board of Internal Medicine (ABIM) Certification from the Blood Pressure Regulation and Hypertension tutorial, as well as points of interest at the end of this document that are not directly addressed in this tutorial but should help you prepare for the boards. See the tutorial notes for further details and relevant links.
 2. Volume regulation:
Below is information not explicitly contained within the tutorial but important for ABIM certification.
2. Volume regulation:
Below is information not explicitly contained within the tutorial but important for ABIM certification.
- --
VITAL FOR ABIM
Pathophysiology of Hypertension
1. Hemodynamic determinants:
- Mean arterial pressure = cardiac output × total peripheral resistance
- Cardiac output = heart rate × stroke volume
- Stroke volume dependent on preload and contractility
- Total peripheral resistance primarily determined by arteriolar tone
 2. Volume regulation:
2. Volume regulation:
- Blood volume directly impacts preload
- Increased venous return elevates cardiac output
- Sodium and water retention by kidneys determines blood volume
- Salt-sensitivity as a clinically significant phenomenon
- Small arteries and arterioles primary determinants of resistance
- Vasoconstriction significantly increases total peripheral resistance
- Vascular remodeling contributes to sustained hypertension
- Balance between vasoconstrictors and vasodilators
Key Mediators in Clinical Context
1. Renin-Angiotensin-Aldosterone System:
- Angiotensin II: potent vasoconstrictor
- Direct effects: increased sodium/water retention
- Indirect effects: stimulates release of norepinephrine, ADH, aldosterone
- Principal target of multiple antihypertensive classes (ACEIs, ARBs)
- Aldosterone: promotes sodium retention and potassium excretion
- Vasopressin (ADH): vasoconstrictor with water retention effects
- Clinical relevance in volume-dependent hypertension
- Norepinephrine increases vasoconstriction, heart rate, and contractility
- Sympathetic hyperactivity as a mechanism in essential hypertension
- Endothelin elevation in remodeled vessels
- Reduced nitric oxide bioavailability
- Imbalance contributes to sustained hypertension
Hypertensive Crisis Management
1. Hypertensive urgency vs. emergency:
- Urgency: BP >180/120 mmHg without end-organ damage
- Emergency: BP >180/120 mmHg with end-organ damage
- Distinction critical for management decisions
- Neurological: severe headache, confusion, vision changes, seizures
- Cardiovascular: chest pain, dyspnea
- Gastrointestinal: nausea, vomiting
- Psychological: anxiety
- --
HIGH YIELD
Clinical Applications of Pathophysiology
1. Therapeutic targeting of RAAS:
- Angiotensin II increases vasoconstriction and sodium/water retention
- ACE inhibitors reduce angiotensin II and increase bradykinin
- Multiple drug classes target different components of this system
- Consideration of complete pathway important for combination therapy
- Salt-sensitive patients respond to sodium restriction and diuretics
- Clinical identification of volume-dependent mechanisms
- Relationship between sodium intake and blood pressure in susceptible individuals
- Aldosterone-secreting tumors present with volume expansion
- Key vasodilators: nitric oxide, prostaglandins, histamine, bradykinin
- Bradykinin degraded by angiotensin II
- Therapeutic implications: medications affecting both systems
- Vascular remodeling alters responsiveness to vasodilators
- Multiple genetic and environmental factors affect BP components
- Screening for underlying causes based on clinical presentation
- Understanding mechanisms guides appropriate testing
- --
Beyond the Tutorial
Evidence-Based Management
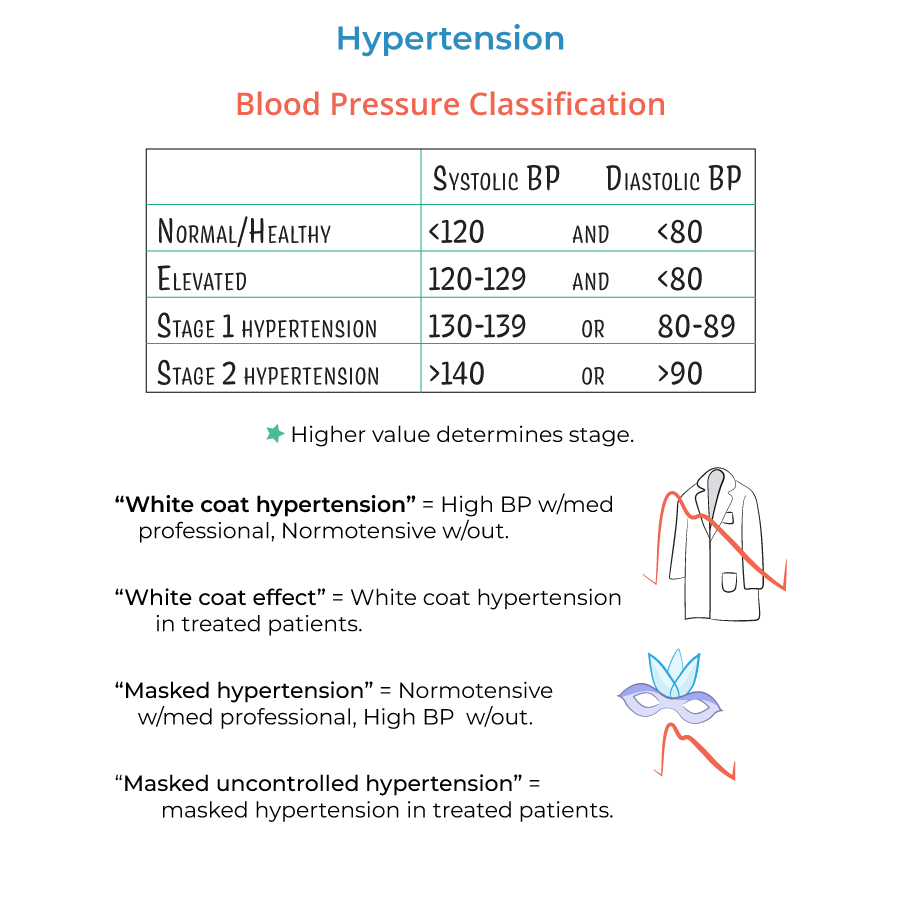
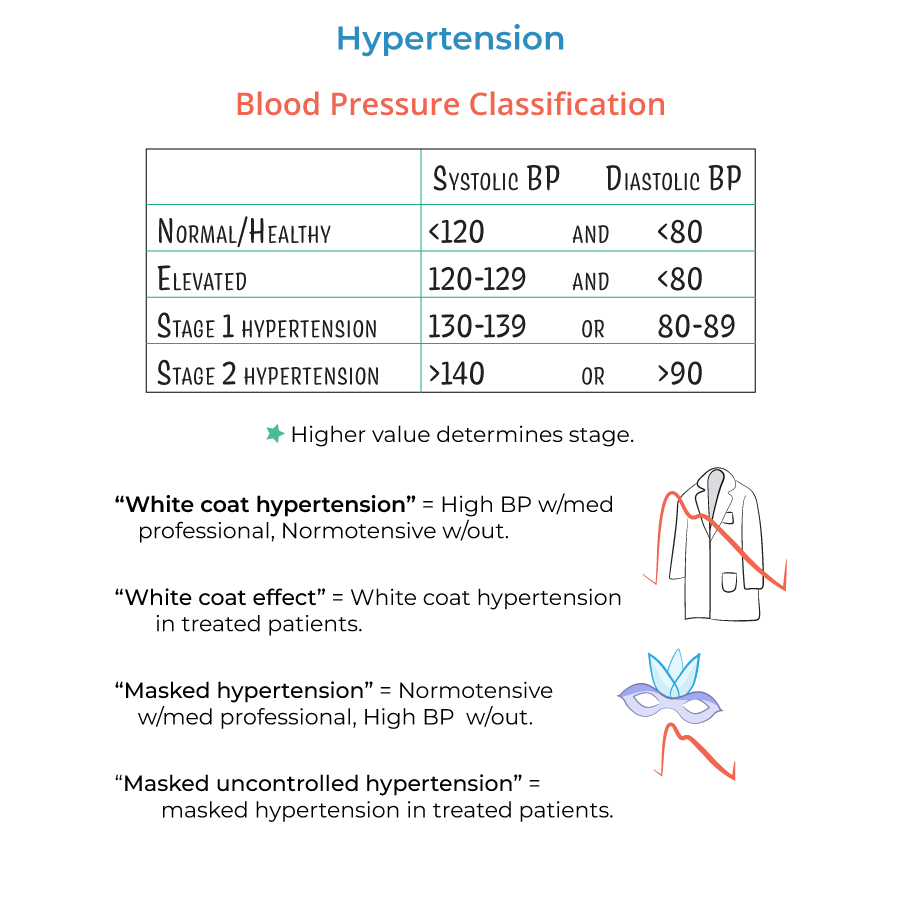
1. Current guideline recommendations:
- Classification of BP categories
- Initial evaluation and risk stratification
- Treatment thresholds and targets
- Monitoring parameters and follow-up intervals
- First-line agents and their mechanisms
- Compelling indications for specific classes
- Combination strategies based on complementary mechanisms
- Management of side effects and complications
- Elderly patients
- Pregnancy
- Diabetes and metabolic syndrome
- Chronic kidney disease
- Heart failure
- Post-stroke
Complex Management Scenarios
1. Resistant hypertension:
- Definition and diagnostic criteria
- Systematic evaluation approach
- Therapeutic strategies
- Consideration of secondary causes
- Hypertensive encephalopathy
- Acute coronary syndromes
- Acute heart failure
- Aortic dissection
- Eclampsia
- Acute kidney injury
- Cardiovascular risk modification
- Target organ damage prevention
- Population-based strategies
- Team-based care models
