ABIM - Endocarditis
Start your One-Week Free Trial
Already subscribed? Log in »
Here are key facts for ABIM from the Endocarditis tutorial, as well as points of interest at the end that are not directly addressed in this tutorial but should help you prepare for the boards. See the tutorial notes for further details and relevant links.
 1. Endocarditis = inflammation of the internal lining of the heart (endocardium).
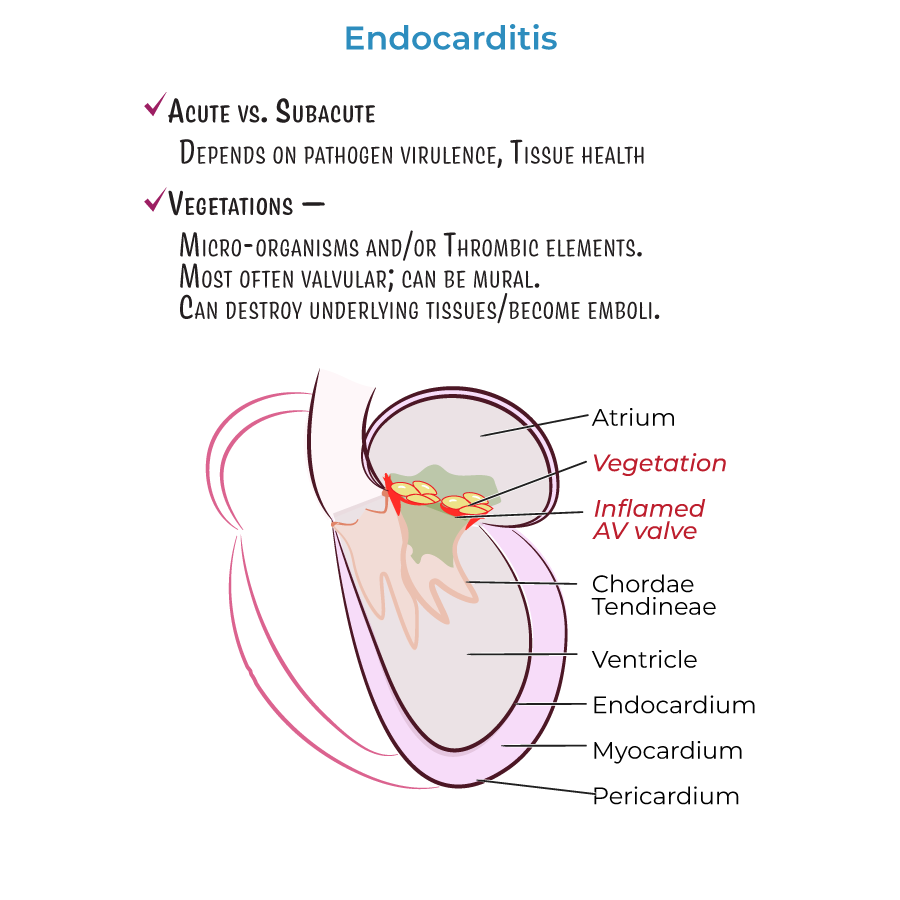
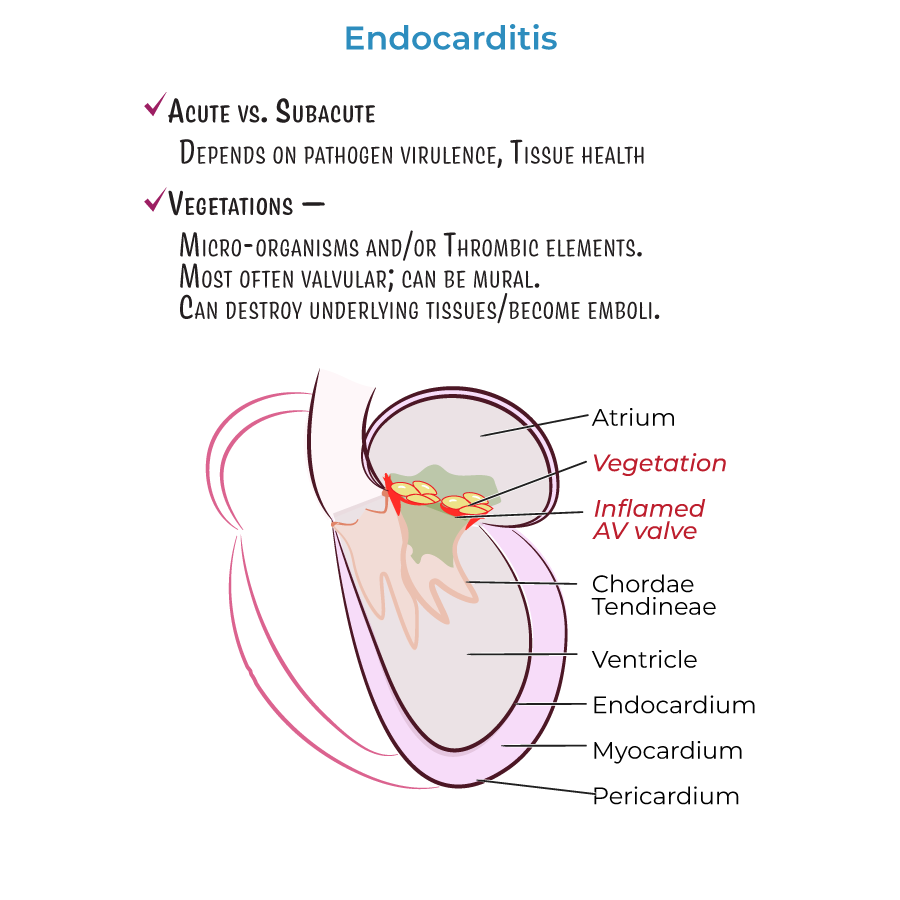
2. Can be acute or subacute, depending on pathogen virulence and cardiac tissue health.
3. Acute endocarditis presents with fever, chills, and other flu-like symptoms.
4. Classification:
1. Endocarditis = inflammation of the internal lining of the heart (endocardium).
2. Can be acute or subacute, depending on pathogen virulence and cardiac tissue health.
3. Acute endocarditis presents with fever, chills, and other flu-like symptoms.
4. Classification:
 Additional information important for ABIM:
Additional information important for ABIM:
- --
VITAL FOR ABIM
Definition and Clinical Approach
 1. Endocarditis = inflammation of the internal lining of the heart (endocardium).
2. Can be acute or subacute, depending on pathogen virulence and cardiac tissue health.
3. Acute endocarditis presents with fever, chills, and other flu-like symptoms.
4. Classification:
1. Endocarditis = inflammation of the internal lining of the heart (endocardium).
2. Can be acute or subacute, depending on pathogen virulence and cardiac tissue health.
3. Acute endocarditis presents with fever, chills, and other flu-like symptoms.
4. Classification:
- Infective endocarditis: Contains pathogens in vegetations
- Non-infective endocarditis: Contains sterile vegetations (marantic or non-bacterial thrombotic)
- Culture-negative endocarditis: Infectious agent present but not identified by routine cultures
Pathophysiology and Complications
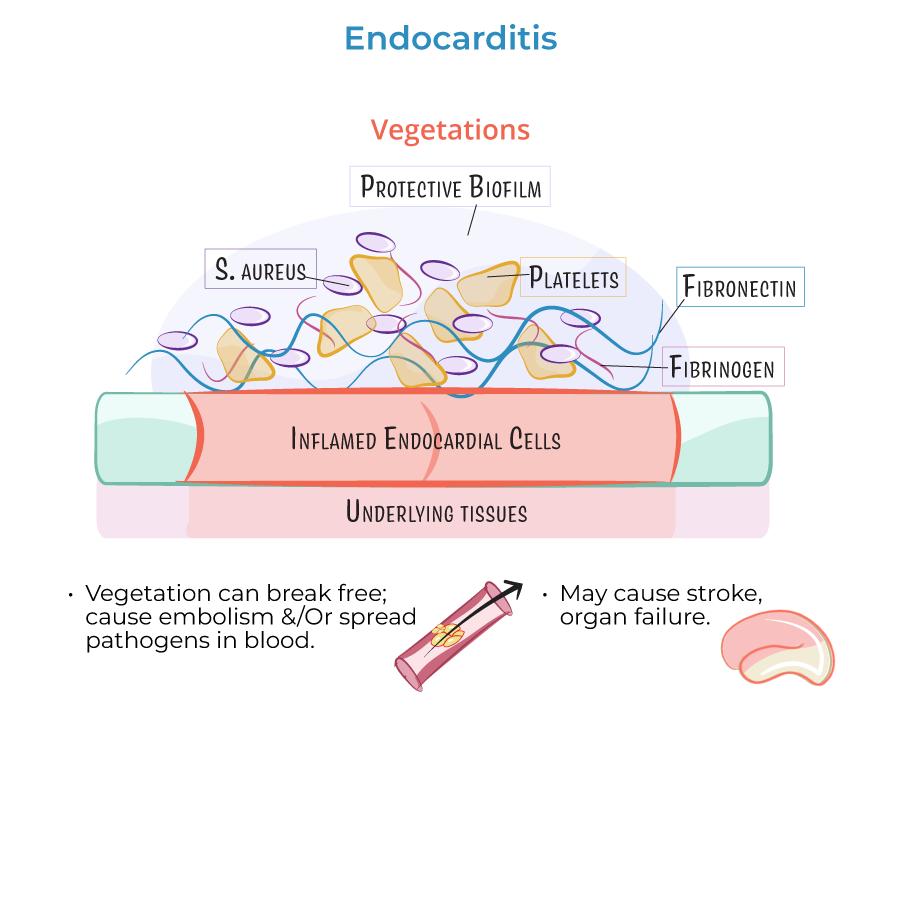
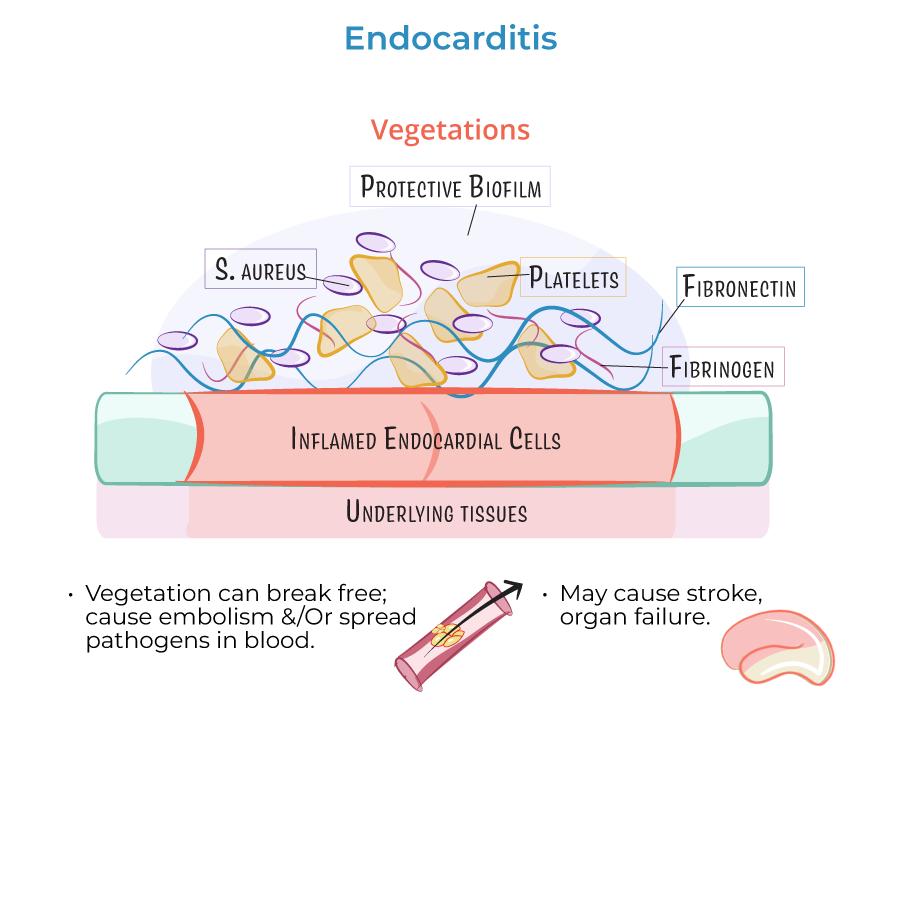
1. Vegetations comprise microorganisms and/or thrombotic elements, primarily on valvular ring or leaflets.
2. Vegetations can invade and destroy underlying tissues or break free and become emboli.
3. Complications include stroke, organ failure, and sepsis when emboli lodge in blood vessels.
Microbiology
1. Gram-positive bacteria most common in infective endocarditis:
- Staphylococcus aureus (most common)
- Viridans group Streptococci
- Enterococci
- Coagulase-negative Staphylococci
- Haemophilus species
- Aggregatibacter species
- Cardiobacterium hominis
- Eikenella corrodens
- Kingella kingae
- --
HIGH YIELD
Risk Factors and High-Risk Populations
1. Valvular damage: Increases likelihood of vegetation formation.
2. Catheter-induced abrasion or prosthetic devices can cause initial inflammation.
3. Intravenous drug use: Major cause of right-sided valvular endocarditis due to:
- Particulate matter (talc) introduction
- Surface pathogens from skin
- Oral bacterial flora (if saliva used on injection needles)
- More susceptible to infection (bacteria adhere to prosthetic materials)
- Surgical/healing process creates vulnerable environment
- Common pathogens: S. aureus and Coagulase-negative Staphylococci
- Often requires surgical valve replacement
Pathophysiology of Vegetation Formation
1. Endothelial damage promotes fibronectin deposition and vegetation formation.
2. Fibronectin adheres to circulating fibrin, platelets, white blood cells, and pathogens.
3. Turbulent blood flow promotes vegetation formation.
4. Vegetation patterns by valve condition:
- Mitral valve regurgitation: Lesions on atrial leaflet surface
- Aortic insufficiency: Vegetations on ventricular side
- Ventricular septal defects: Right-sided vegetations near orifice
- Rheumatic heart disease: Small vegetations near edge of leaflet
Special Clinical Considerations
1. Libman-Sacks endocarditis:
- Associated with Systemic Lupus Erythematosus
- Small/medium vegetations on both sides of leaflets
- Less inflammation means vegetations are loosely attached
- Increased risk of embolism
- Invasive vegetations where prosthetic annular ring meets tissue
- Can deform valvular leaflets
- Surgery often required to replace valve
- --
Beyond the Tutorial
Diagnostic Evaluation
1. Modified Duke criteria: Definitive diagnosis requires:
- 2 major criteria, or
- 1 major + 3 minor criteria, or
- 5 minor criteria
- Minimum 3 sets from different sites
- Drawn before antibiotic initiation
- Extended incubation for difficult organisms
- TTE: First-line, sensitivity ~60-65%
- TEE: Higher sensitivity (~90-95%), especially for prosthetic valves
- Elevated inflammatory markers (ESR, CRP)
- Normocytic anemia
- Microscopic hematuria
- Positive rheumatoid factor
Treatment Strategy
1. Antimicrobial therapy:
- Empiric coverage based on Gram stain, valve type, clinical scenario
- Prolonged IV therapy (4-6 weeks for native valves, 6-8 weeks for prosthetic)
- Synergistic combinations for resistant organisms
- Therapeutic drug monitoring
- Heart failure due to valvular dysfunction
- Uncontrolled infection (persistent bacteremia, abscess)
- Recurrent emboli or large mobile vegetations
- Prosthetic valve dehiscence
- Fungal endocarditis
- Emergency: Severe CHF, valvular obstruction, abscess
- Urgent: Heart failure, persistent infection, large vegetations
- Elective: Based on progress and risk assessment
Prevention
1. Antibiotic prophylaxis: Limited to highest-risk patients:
- Prosthetic valves
- Previous endocarditis
- Unrepaired cyanotic congenital heart disease
- Repaired CHD with residual defects
- Dental hygiene
- Substance use disorder treatment
- Aseptic technique for vascular access
