ABIM - Atherosclerosis
Start your One-Week Free Trial
Already subscribed? Log in »
Here are key facts for ABIM from the Atherosclerosis Tutorial, as well as points of interest at the end of this document that are not directly addressed in this tutorial but should help you prepare for the boards. See the tutorial notes for further details and relevant links.
- --
VITAL FOR ABIM
Disease Process and Complications
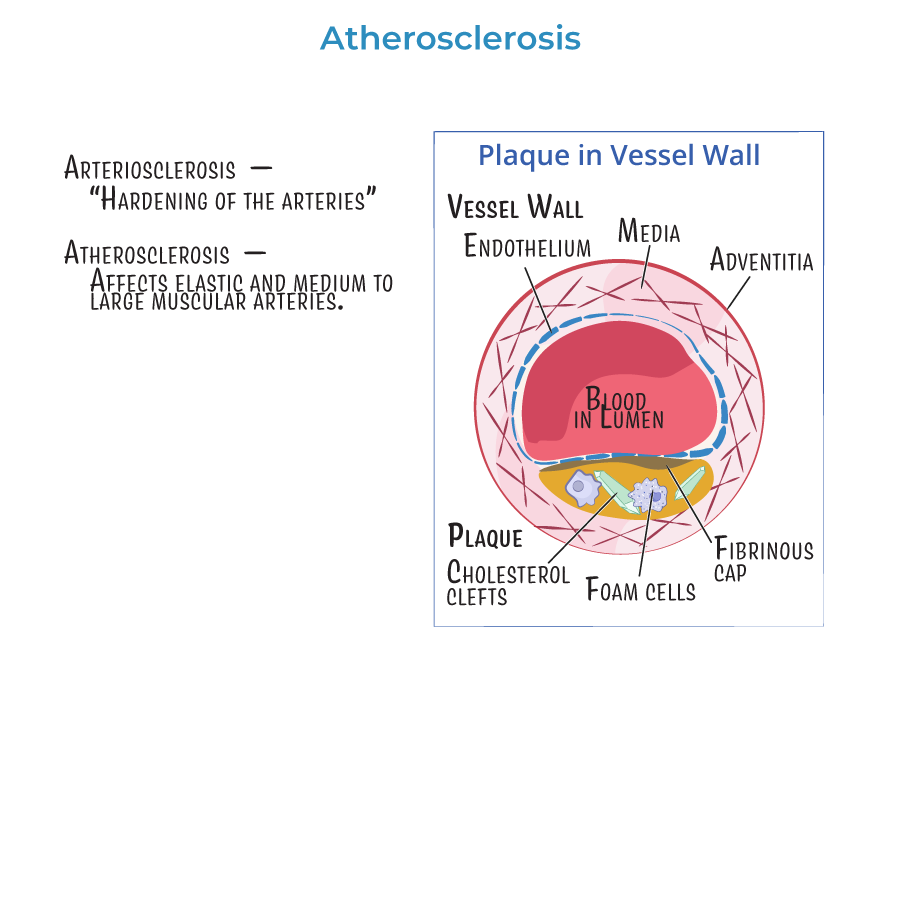
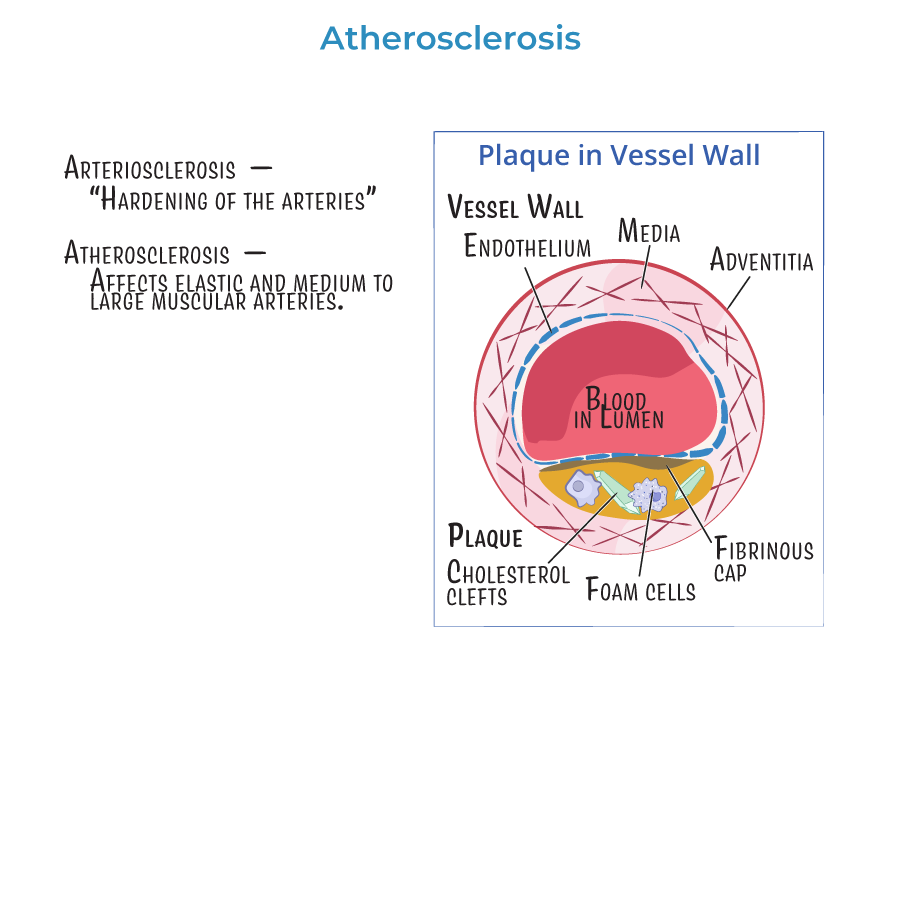
1. Atherosclerosis is the pathologic basis for major cardiovascular diseases: coronary artery disease (CAD), stroke, peripheral artery disease (PAD), and aortic aneurysms.
2. It begins with endothelial injury, followed by lipid deposition, inflammation, and fibrous plaque formation.
3. Clinical events like myocardial infarction, unstable angina, ischemic stroke, and acute limb ischemia result from plaque rupture and thrombosis.
4. PAD presents with claudication, poor wound healing, and in advanced cases, critical limb ischemia or gangrene.
5. Coronary artery disease presents with angina, dyspnea, or acute coronary syndrome.
Risk Assessment and Prevention
6. Use the ASCVD 10-year risk calculator in adults age 40–75 to guide primary prevention strategies.
7. High-intensity statins (e.g., atorvastatin 40–80 mg, rosuvastatin 20–40 mg) are indicated in:
- Clinical ASCVD
- LDL ≥190 mg/dL
- Age 40–75 with diabetes and LDL ≥70 mg/dL
- ASCVD risk ≥7.5%
Follow-Up and Targets
9. Lipid panel should be checked 4–12 weeks after statin initiation, then every 6–12 months.
10. Target LDL reduction is ≥50% for high-intensity statins and 30–49% for moderate-intensity statins.
11. If LDL remains ≥70 mg/dL despite maximally tolerated statin, add ezetimibe; PCSK9 inhibitors may be considered for very high-risk patients.
- --
HIGH YIELD
Diagnostics
1. ABI < 0.90 is diagnostic for PAD; use it in patients with claudication or diminished pulses.
2. Carotid duplex ultrasound is appropriate for asymptomatic bruits or stroke evaluation.
3. Coronary artery calcium (CAC) score helps stratify intermediate-risk patients.
4. CT angiography or MRA is used for aortic aneurysm and dissection evaluation.
Additional Risk Factors and Labs
5. Non-modifiable risks: age, male sex, family history of premature CVD.
6. Modifiable risks: smoking, hypertension, hyperlipidemia, diabetes, obesity, sedentary lifestyle.
7. Consider checking hs-CRP for inflammation-based risk stratification in borderline cases.
8. Monitor HbA1c, fasting glucose, and BP as part of cardiovascular risk control.
Lifestyle Modification
9. Emphasize:
- Smoking cessation
- Heart-healthy diet (e.g., Mediterranean or DASH)
- Exercise: ≥150 min/week moderate aerobic activity
- Weight management and BMI <25
Medication Considerations
11. Statin side effects include myopathy, transaminitis, and rare rhabdomyolysis.
12. For muscle-related symptoms, check CK and consider dose reduction or switch to alternative statin.
13. Avoid simvastatin with protease inhibitors, macrolides, or grapefruit juice.
14. Statins are not contraindicated in liver disease unless LFTs are ≥3x ULN and symptoms are present.
- --
Beyond the Tutorial
Special Populations
1. Diabetics age 40–75 should receive moderate or high-intensity statins regardless of ASCVD risk.
2. Chronic kidney disease patients not on dialysis benefit from statin-based risk reduction.
3. HIV-positive patients have elevated ASCVD risk and may need earlier or more aggressive management.
4. Patients with inflammatory diseases (e.g., lupus, rheumatoid arthritis) are at higher atherosclerotic risk.
Clinical Reasoning
5. A patient with normal LDL but multiple risk factors (e.g., HTN, smoking, family history) may still benefit from statin therapy.
6. Statin re-challenge is appropriate after discontinuation for mild side effects, starting with low dose and slow titration.
7. Do not initiate aspirin for primary prevention in patients without diabetes or known ASCVD unless risk is ≥10% and bleeding risk is low.
8. Avoid overtreatment: very low LDL (<40 mg/dL) may increase hemorrhagic stroke risk in older adults.
Management Sequencing
9. In high-risk patients, if LDL goal is not met:
- First, confirm adherence and lifestyle changes.
- Then, add ezetimibe.
- If still not at goal, consider PCSK9 inhibitor.
