ABIM - Aortic Aneurysm & Dissection
Start your One-Week Free Trial
Already subscribed? Log in »
Here are key facts for ABIM from the Aortic Aneurysm & Dissection, as well as points of interest at the end of this document that are not directly addressed in this tutorial but should help you prepare for the boards. See the tutorial notes for further details and relevant links.

- --
VITAL FOR ABIM
Aortic Aneurysm
1. Abdominal Aortic Aneurysm (AAA) screening is recommended for men aged 65–75 who have ever smoked, with one-time abdominal ultrasound.
2. AAA is diagnosed when the abdominal aortic diameter exceeds 3.0 cm.
3. Elective repair is indicated for AAA size ≥5.5 cm, rapid expansion (>0.5 cm in 6 months), or if symptomatic.
4. Symptomatic AAAs, regardless of size, require emergency surgical repair.
5. Risk factors for AAA include male gender, age >65, smoking, hypertension, and atherosclerosis.
6. Smoking cessation is critical to slow aneurysm progression and should be actively counseled.
7. Thoracic aortic aneurysms are associated with genetic conditions such as Marfan syndrome, Ehlers-Danlos, and Loeys-Dietz syndromes.
8. Surgical repair for thoracic aneurysms is recommended at ≥5.5 cm or sooner in patients with genetic disorders.

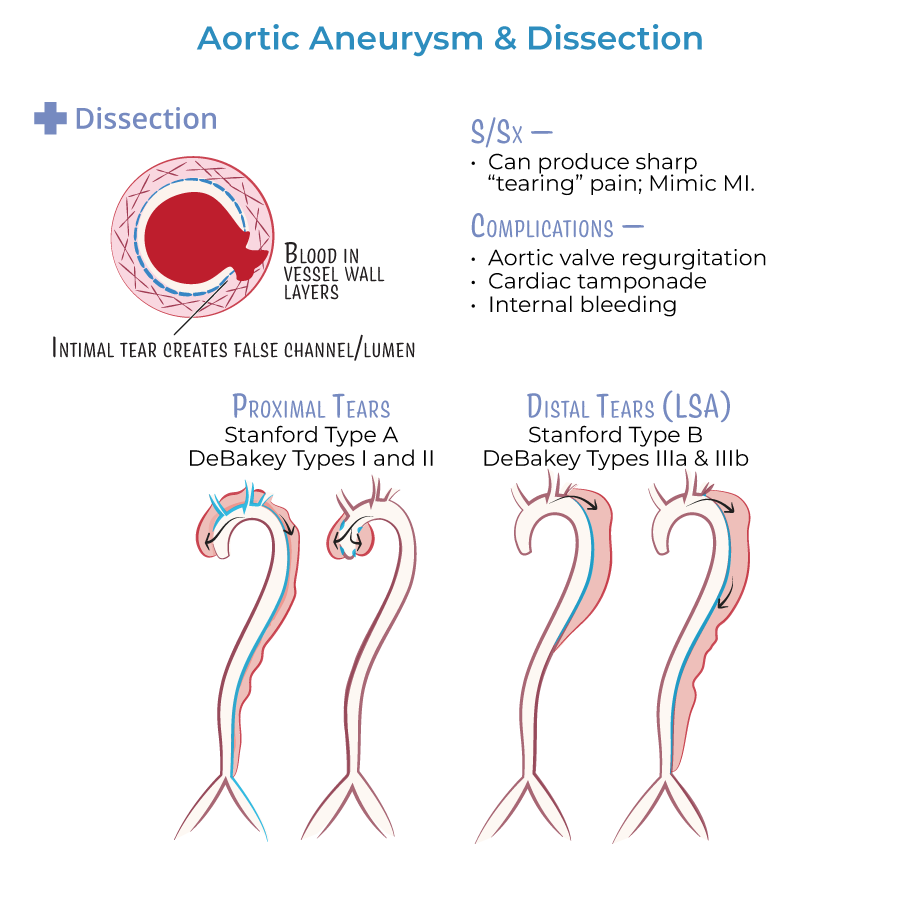
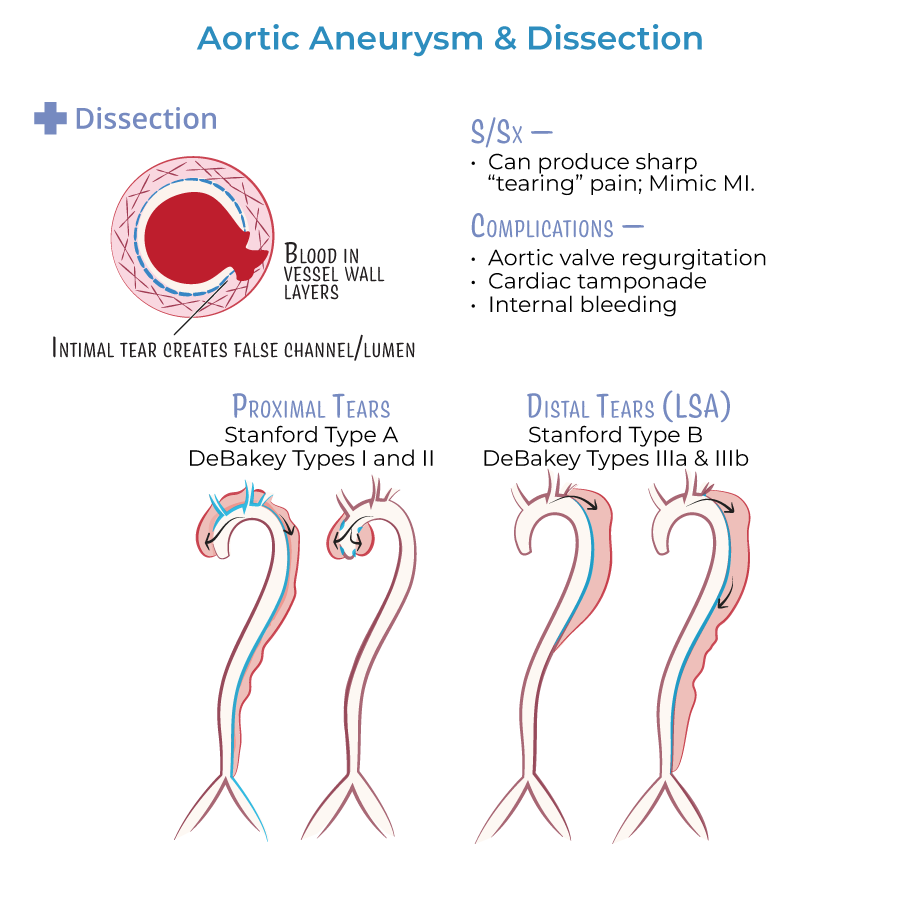
Aortic Dissection
9. Stanford Type A dissection (ascending aorta) is a surgical emergency.
10. Stanford Type B dissection (descending aorta) is managed medically first unless there are complications such as rupture or malperfusion.
11. The classic presentation of dissection is sudden onset, tearing chest or back pain, often with pulse deficits or blood pressure differences between limbs.
12. CT angiography is the gold standard imaging for stable patients; transesophageal echocardiography (TEE) is used for unstable patients.
13. Initial management includes IV beta-blockade (e.g., esmolol) to reduce shear forces before adding vasodilators if needed.
14. Goal heart rate is less than 60 bpm and systolic blood pressure less than 120 mmHg.
- --
HIGH YIELD
Etiology and Pathophysiology
1. Hypertension is the most important risk factor for aortic dissection.
2. Smoking is the strongest modifiable risk factor for AAA formation and expansion.
3. Atherosclerosis is strongly associated with abdominal aneurysms.
4. Cystic medial degeneration is the underlying pathology in thoracic aneurysms and dissections.
Clinical Features
5. Chest x-ray in aortic dissection may show widened mediastinum.
6. AAA rupture presents with abdominal or back pain, hypotension, and a pulsatile abdominal mass.
7. Dissection into the coronary arteries may mimic myocardial infarction.
8. Aortic regurgitation may result from Type A dissection involving the aortic valve.
9. Stroke, mesenteric ischemia, and renal failure can result from dissection involving branch arteries.
10. Thoracic aneurysms may present with dysphagia, hoarseness, or cough due to mass effect.
11. Pain that migrates suggests extension of the dissection.
Diagnostics
12. MRI angiography is an alternative in patients with contraindications to contrast or in elective settings.
13. Bedside TEE is best for unstable patients when immediate imaging is necessary.
Pharmacology
14. Fluoroquinolones are associated with increased risk of aortic aneurysm rupture and should be avoided in high-risk individuals.
15. Long-term blood pressure control is essential post-dissection or aneurysm repair to prevent recurrence.
- --
Beyond the Tutorial
Risk Stratification and Long-Term Management
1. Stanford Type A dissection requires emergent surgical intervention regardless of symptoms.
2. Stanford Type B dissection patients who are stable are treated with beta-blockers and monitored closely.
3. Post-repair surveillance involves periodic CT or MRI imaging every 6 to 12 months.
4. Annual follow-up with imaging is required for thoracic aneurysms that have not yet met surgical criteria.
5. Beta-blockers are first-line to manage hypertension in Marfan patients to slow aortic root dilation.
Emergency Medicine and Critical Care
6. In shock with a pulsatile mass, presume ruptured AAA and transfer to OR immediately without waiting for imaging.
7. Hypotension in the setting of acute chest pain and widened mediastinum should raise strong suspicion for aortic rupture or tamponade.
8. Surgery vs medical management decisions in dissection are critical and based primarily on anatomic location (Type A vs Type B).
9. Pain control is crucial to lower sympathetic drive and reduce further propagation of dissection.
