Start your One-Week Free Trial
Already subscribed? Log in »
Osteoporosis
Definition
Osteoporosis is a disease of excessive bone resorption (bone loss).
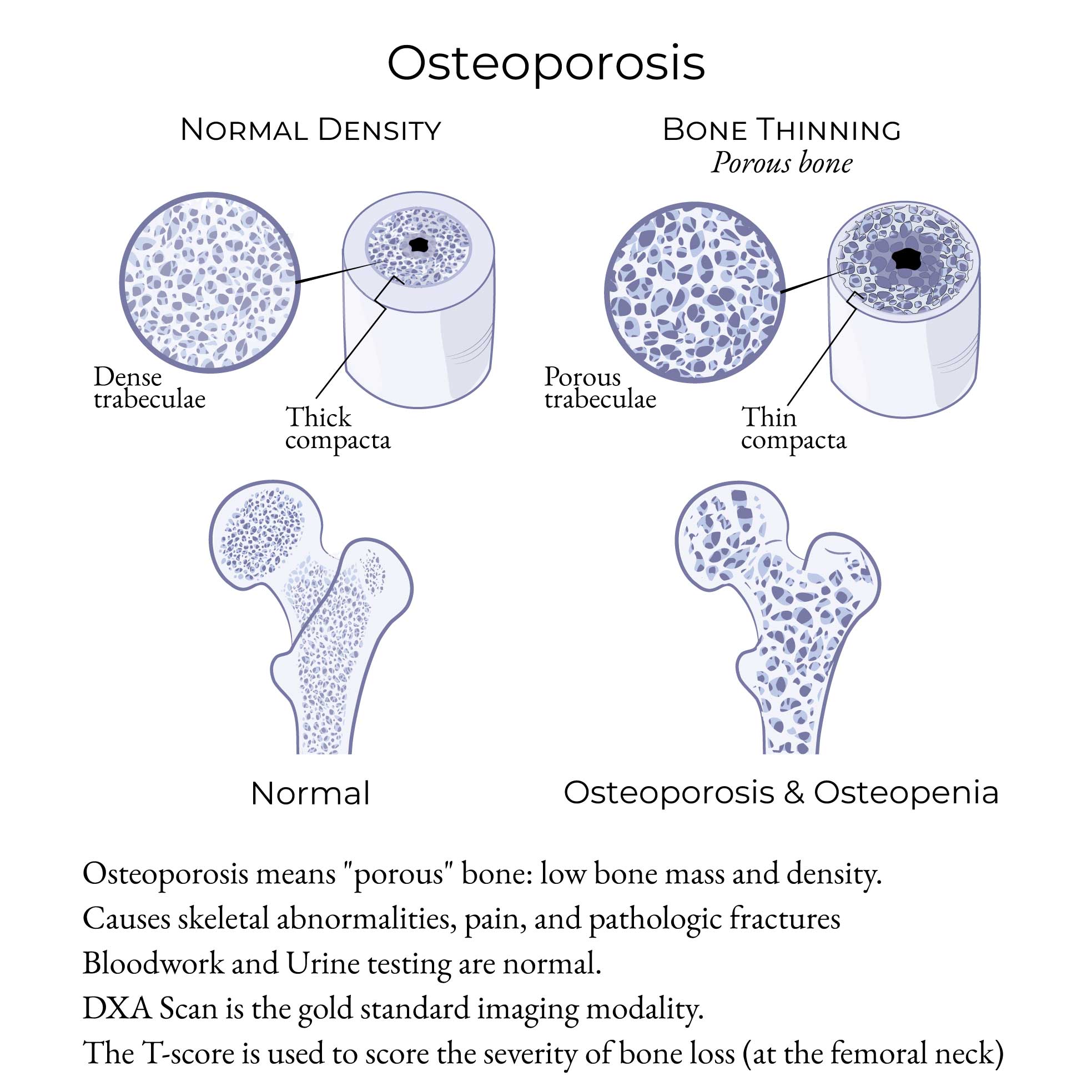
In essence, the trabecular bone hollows-out: the trabecular network becomes discontinuous (interrupted), and the trabeculae shrink and disappear.
It first impacts trabecular bone because trabecular bone is less dense (spongier) than cortical bone.
Eventually, the cortical bone also thins-out and becomes more porous.
Histopathology
General Bone Anatomy: Trabecular vs Cortical Bone
In brief, bones have varying concentrations of trabecular (aka cancellous, spongy) bone and cortical (compact) bone. There is a high proportion of trabecular bone in the vertebral bodies and also the ends of the long bones (the metaphyses and epiphyses). Whereas, the dense outer layer of the long bones is cortical bone, and the long bone shaft (the diaphysis) is primarily cortical bone. The center of the diaphysis from a trabecular network to a marrow cavity during fetal development.
Pathogenesis
Osteoporosis is a disease of excessive bone resorption (bone loss). It first impacts trabecular bone because trabecular bone is, by nature, less dense (spongier) than cortical bone.
Put technically: trabecular bone has a high surface area to bone cell ratio. This is why the femoral neck (which has a high proportion of trabecular bone) is used to identify the severity of bone loss.
The trabecular bone hollows-out: the trabecular network becomes discontinuous (interrupted), and the trabeculae shrink and disappear.
The cortical bone eventually thins-out and becomes more porous.
Osteopenia vs Osteoporosis
The T-score is a measurement of bone density (bone mass) as it compares to a young healthy adult (a premenopausal woman). Bone density is calculated using a low-dose X-ray DXA Scan (aka DEXA (dual-energy X-ray absorptiometry) scan) at the femoral neck (standard site).
T-score Measurements
- Normal: -1.0 to 0
- Osteopenia: -1.0 to -2.5
- Osteoporosis: < -2.5
Pathogenesis
Histopathological findings
- Cortical thinning and weakening (increased porosity)
- Trabecular network disruption
- The vertebral bodies and the ends of the long bones (eg, the femoral neck) have substantial trabecular bone.
- Note that the T-score is measured at the femoral neck.
- The bulk of the long bones (eg, the femur, tibia, humerus) have greater cortical bone.
Clinical Symptoms/Signs
- Loss of height due to vertebral bone collapse
- Back pain due to vertebral compression fractures
- Kyphosis and Stooped posture
- Increased risk of fractures, particularly in the wrist, hip, and spine (sites of high trabecular to cortical bone ratio).
- Pathologic bone fractures, which are fractures that occur with minimal trauma, such as a fall from a standing height (vertebral fractures (thoracic, lumbar) compression fractures and long bone fractures).
Imaging Modalities
DXA Scan
DXA Scan (aka DEXA (dual-energy X-ray absorptiometry) scan) is the gold standard test for bone density measurement.
- DXA is used to detect current severity of bone loss (osteopenia vs osteoporosis) and the later risk for osteoporosis.
- Rate of bone loss via sequential measurements (over time).
- Efficacy/Failure of therapy.
- Improves therapy compliance (the practical impact of patients repeatedly undergoing DXA Scans is that both the patient and the clinical provider pay closer attention to the treatment plan).
- It is a cost effect, noninvasive, quick, low radiation, broad, reliable, standardized imaging tool and thus is considered the gold standard for assessment.
Other Modalities
X-Rays are unable to detect early changes of osteoporosis but can reveal prior fractures and other secondary characteristics of bone loss.
Bone scan (99mTc-labelled bisphosphonate) can detect bone lesions and fractures, due to increased uptake at pathological sites (sites of fracture, degeneration, inflammation, and malignancy).
CT scan requires high resolution imaging and high radiation exposure to be of use in assessment of osteoporosis.
MRI is best suited for soft tissue evaluation, such as detection of mass lesion, marrow assessment, and distinguishing fracture from metastasis.
Asymptomatic Screening
Some considerations for asymptomatic screening are:
- Perimenopausal women ready to start drug therapy.
- Radiographic evidence of bone loss.
- Patients who have been on chronic steroids.
- Asymptomatic hyperparathyroidism.
Risk Factors
Key Risk Factors include:
- Deficiencies in calcium and vitamin D and excess parathyroid hormone are problematic – there are numerous causes for these deficiencies and for hyperparathyroidism.
- Postmenopausal women have a reduction in estrogen that leads to accelerated bone loss via increase in bone resorption at a faster pace than bone formation.
- Genetic factors play a key role, as well, especially RANKL, which is a specific therapeutic target.
- Two key modifiable risk factors are tobacco abuse and glucocorticoid (ie, steroid) administration.
Laboratory Testing
Serologies and urine labs are normal in primary osteoporosis.
A broad range of labs are used to look for secondary causes (including, but not limited to):
- CBC
- CMP to assess Creatinine, Calcium, Phosphorous, Glucose, AST, ALT, Alkaline phosphatase
- ESR and/or CRP
- Thyroid studies and Parathyroid studies
- Estrogen and Testosterone levels
- Vitamin D and Vitamin K
- SPEP and Immunofixation panel
Treatment
The treatment of osteoporosis involves a multifaceted approach aimed at reducing the risk of fractures and improving bone health. Some of the common treatment strategies include:
1. Lifestyle modifications: Regular exercise, particularly weight-bearing and strength training exercises, can help maintain and improve bone density. Adequate intake of calcium and vitamin D is also essential for bone health.
2. Calcium with vitamin D supplementation
3. Medications: Several medications can help slow bone loss, increase bone density, and reduce the risk of fractures.
- Bisphosphonates ("-dronates" (eg, alendronate))
- Denosumab (RANKL inhibitor)
- Estrogen replacement therapy (estrogen insufficiency leads to bone loss)
- Selective estrogen receptor modulators (eg, raloxifene)
- Teriparatide (human PTH analog (risk of osteosarcoma))
